Abstract [View PDF] [Read Full Text]
Objective
To assess the effectiveness of Vision Therapy System 4 (VTS4) combined with traditional comprehensive training for ametropic amblyopia.
Methods
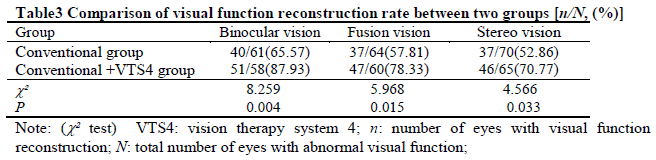
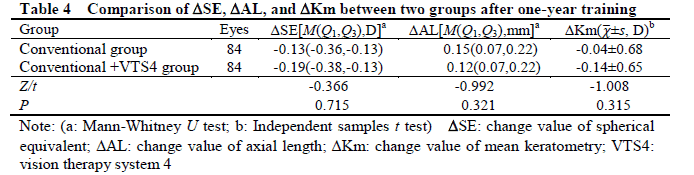
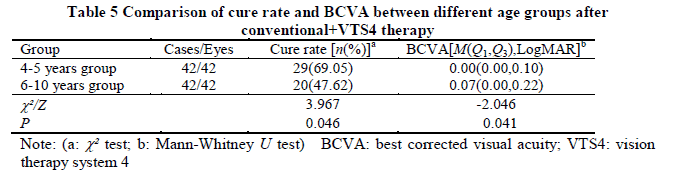
A non-randomized controlled clinical study was performed.A total of 168 children aged 4-10 years with ametropic amblyopia were enrolled in The First Affiliated Hospital of Zhengzhou University from January 2018 to March 2021.The children were assigned to conventional comprehensive training combined with Vision Therapy System 4 group (conventional+ VTS4 group) and conventional group according to the preference of their guardian.Patients in conventional+ VTS4 group (84 children) received conventional comprehensive training combined VTS4 and patients in conventional group (84 children) were treated with conventional comprehensive training only, and the intervention was continuously used for over a year.Best corrected visual acuity (BCVA) of the patients converted to the logarithm of the minimum angle of resolution (LogMAR) units was examined by international standard visual acuity chart before and after therapy.Spherical equivalent of the patients was detected by optometry under cycloplegic conditions and skiascopy.Binocular and fusion vision was examined with a synoptiscope.The stereopsis was evaluated using Titmus Stereogram.The ocular axial length (AL) and mean keratometry (Km) were measured with the IOLMaster 500.The basic cure rate, BCVA, reconstruction rate of stereopsis, △SE, △AL and △Km following training were compared to evaluate the effectiveness and myopic shift between two groups.The patients in conventional+ VTS4 group were divided into 4-5 years old group and 6-10 years old group, with 42 cases in each group, and the basic cure rate, BCVA, reconstruction rate of stereopsis were compared to evaluate the therapeutic effect between the two groups.The basic cure was defined as acuity improved to ≥0.9, with reduced myopic diopter and stable therapy outcome over 6 months.This study adhered to the Declaration of Helsinki.The study protocol was approved by an Ethics Committee of The First Affiliated Hospital of Zhengzhou University (No.2021-KY-0891-002). Written informed consent was obtained from guardians prior to any medical examination.
Results
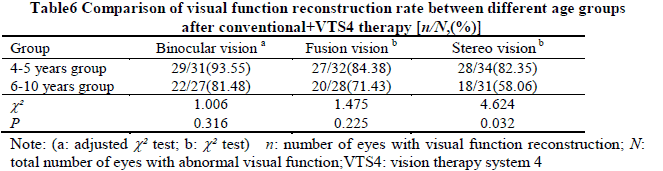
The basic cure rate of conventional+ VTS4 group was 58.33%(49/84), which was significantly higher than 40.48%(34/84) of conventional group (χ2=5.358, P=0.021). The BCVA in the conventional+ VTS4 group was better than that in conventional group, showing a statistically significant difference (Z=-2.537, P=0.011). The recovery rates of binocular vision, fusion vision and stereo vision were 87.93%(51/58), 78.33%(47/60) and 70.77%(46/65) in conventional+ VTS4 group, which were higher than 65.57%(40/61), 57.81%(37/64) and 52.86%(37/70) in conventional group, respectively, with significant differences between them (χ2=8.259, 5.968, 4.566; all at P<0.05). No significant difference was found in △SE, △AL, and △Km between conventional group and conventional+ VTS4 group (all at P>0.05). The basic cure rate was 69.05%(29/42) in the children aged 4-5 years group, which was higher than 47.62%(20/42) in 6-10 years group, respectively, showing a significant difference (χ2=3.967, P=0.046). Both BCVA and the stereo vision recovery rate in the 4-5 years old group were better than those in the 6-10 years old group (Z=-2.046, P=0.041; χ2=4.624, P=0.032).
Conclusions
A combination therapy of VTS4 and conventional comprehensive training can improve the visual acuity and reconstruct the fusion and stereopsis of children with ametropic amblyopia, without causing additional myopic drift.
Key words:
Figures and tables 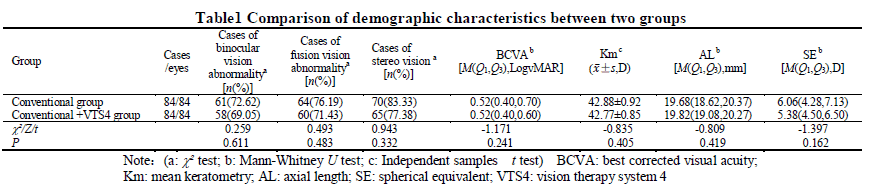

Contributor Information
Department of Ophthalmology, The First Affiliated Hospital of Zhengzhou University, Children’s Eye Disease Prevention and Control Engineering Research Center of Henan Province, Zhengzhou 450052, China
Department of Ophthalmology, The First Affiliated Hospital of Zhengzhou University, Children’s Eye Disease Prevention and Control Engineering Research Center of Henan Province, Zhengzhou 450052, China
Department of Ophthalmology, The First Affiliated Hospital of Zhengzhou University, Children’s Eye Disease Prevention and Control Engineering Research Center of Henan Province, Zhengzhou 450052, China
Department of Ophthalmology, The First Affiliated Hospital of Zhengzhou University, Children’s Eye Disease Prevention and Control Engineering Research Center of Henan Province, Zhengzhou 450052, China
Department of Ophthalmology, The First Affiliated Hospital of Zhengzhou University, Children’s Eye Disease Prevention and Control Engineering Research Center of Henan Province, Zhengzhou 450052, China