Abstract 【Download PDF】 【Read Full Text】
Objective
To compare ocular surface dry eye-related indexes and tear cytokine level changes in chronic ocular graft-versus-host disease (oGVHD) patients after receiving topical treatment of 0.05% cyclosporine or 0.1% tacrolimus eye drops.
Methods
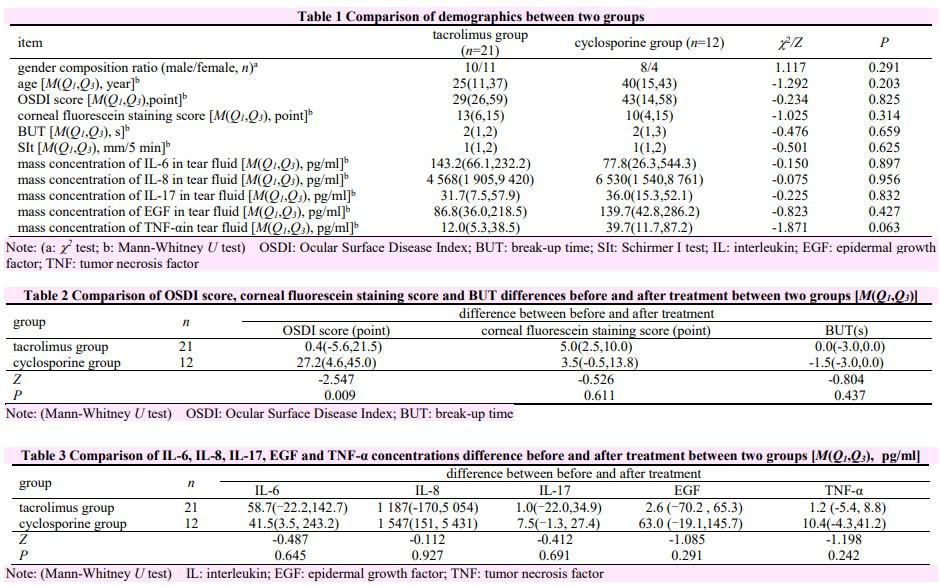
A randomized controlled study was conducted.A total of 60 chronic oGVHD patients (60 eyes) were recruited at Beijing University Third Hospital from April 2020 to April 2021.The patients were divided into tacrolimus group and cyclosporine group by a random number table, with 30 patients (30 eyes) in each group.Patients in tacrolimus group used 0.1% tacrolimus eye drops (twice a day) and patients in cyclosporine group used 0.05% cyclosporine eye drops (4 times a day).Additionally, 0.1% flumetholon (twice a day), deproteinized calf blood extract (3 times a day), and 0.1% sodium hyaluronate eye drops (8 times a day) were applied for anti-inflammation and lubrication in both groups.Patients were screened according to exclusion criteria after 1-month treatment.Eventually, 21 patients (21 eyes) in tacrolimus group and 12 patients (12 eyes) in cyclosporine group were included for further study.Patients were examined before and 1 month after treatment.The primary evaluation indexes included Ocular Surface Disease Index (OSDI), corneal fluorescein staining scores and tear film break-up time (BUT).Expressions of interleukin (IL)-6, IL-8, IL-17, epidermal growth factor (EGF), and tumor necrosis factor-α (TNF-α) in tears were detected before and after treatment using Luminex chip.This study adhered to the Declaration of Helsinki.The study protocol was approved by the Ethics Committee of Peking University Third Hospital (No.M2020489).Written informed consent was obtained from each subject before any medical examination.
Results
The OSDI differences between before and after treatment were 0.4(-5.6, 2.5) in tacrolimus group and 27.2(4.6, 45.0) in cyclosporine group, and the OSDI improvement was significantly greater in cyclosporine group than in tacrolimus group (Z=-2.547, P=0.009).The differences of corneal fluorescein staining scores and BUT between before and after treatment were 5.0(2.5, 10.0) scores and 3.5(-0.5, 13.8) seconds in tacrolimus group, 0.0(-3.0, 0.0) scores and -1.5(-3.0, 0.0) seconds in cyclosporine group, respectively, with no significantly difference between both groups (Z=-0.526, -0.804; both at P>0.05).The differences of IL-6, IL-8, IL-17, EGF and TNF-α expressions between before and after treatment in tacrolimus group and cyclosporine group were not significantly different (Z=-0.487, -0.112, -0.412, -1.085, -1.198; all at P>0.05).
Conclusions
Altered levels of all tested cytokines in oGVHD tears are of no significant differences between tacrolimus and cyclos porine treatment.In addition, 0.05% cyclosporine eye drops may be more comfortable than 1% tacrolimus for chronic oGVHD patients.
Key words:
Figures&Tables
Contributor Information
Department of Ophthalmology, Peking University Third Hospital, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Beijing 100191, China
Department of Ophthalmology, Peking University Third Hospital, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Beijing 100191, China
Department of Ophthalmology, Peking University Third Hospital, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Beijing 100191, China
Department of Ophthalmology, Peking University Third Hospital, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Beijing 100191, China
Department of Ophthalmology, Peking University Third Hospital, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Beijing 100191, China
Department of Ophthalmology, Peking University Third Hospital, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Beijing 100191, China
Wu Rong is working at Department of Ophthalmology, Peking University Shenzhen Hospital, Shenzhen 518000, China
Department of Ophthalmology, Peking University Third Hospital, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Beijing 100191, China
Department of Ophthalmology, Peking University Third Hospital, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Beijing 100191, China