Abstract [View PDF] [Read Full Text]
Objective
To observe the corneal morphology and visual quality after transepithelial photorefractive keratectomy (Trans-PRK) with smart pulse technique (SPT) and 1 050 Hz cutting frequency in the correction of myopia and astigmatism.
Methods
A self-controlled case series study was conducted.Sixty five eyes of 33 patients who underwent Trans-PRK surgery in Ineye Hospital of Chengdu University of TCM from July 2017 to June 2018 were followed up for 6 months.The uncorrected visual acuity (UCVA) converted to logarithm of the minimum angle of resolution (LogMAR) unit, best corrected visual acuity (BCVA) (LogMAR), and spherical equivalent (SE) of the subjects were recorded.The anterior corneal surface symmetry index (SI), the anterior corneal surface Q value in the range of 6, 7, 8, and 9 mm diameter, the spherical aberration, coma, trefoil and total higher-order aberration of the anterior corneal surface, the strehl ratio (SR), and the modulation transfer function (MTF) of 10, 20, 30, and 40 c/d in the horizontal and vertical meridian directions before and after surgery were measured with Sirius corneal topography analyzer.The differences of each index among different time points were compared, and the correlation between indexes was analyzed by Pearson correlation analysis.This study followed the Declaration of Helsinki.The study protocol was approved by the Medical Ethics Committee of Ineye Hospital of Chengdu University of TCM (No.2020yh-004). All patients signed the informed consent form before surgery.
Results
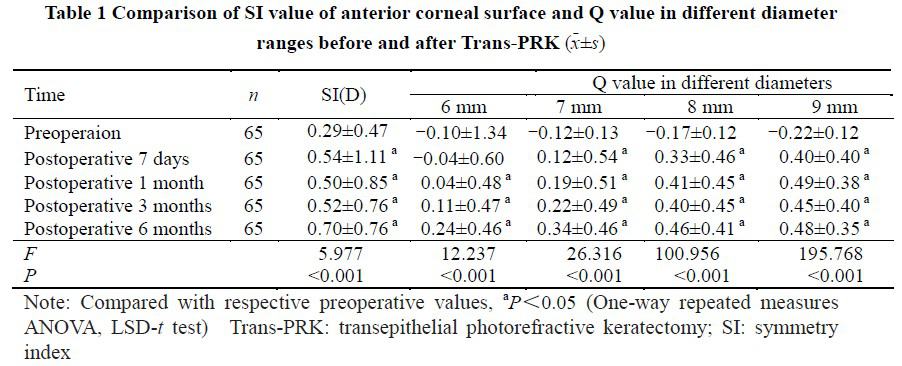
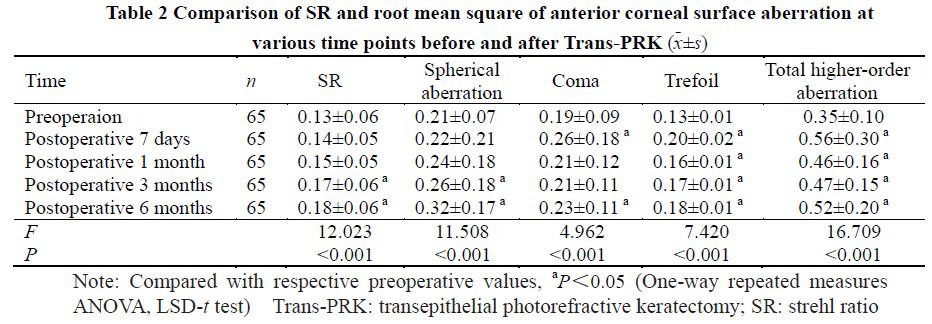
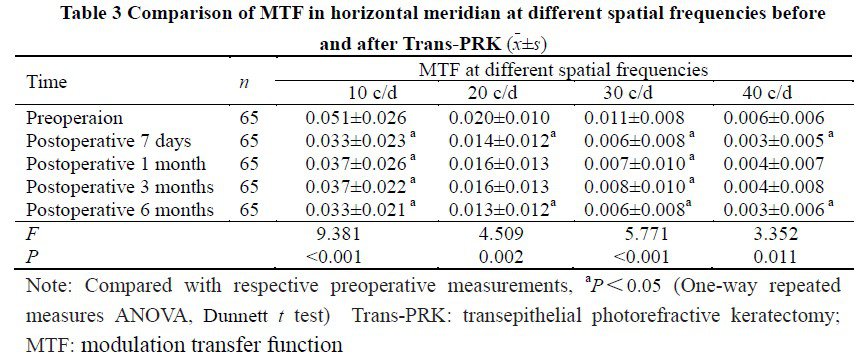
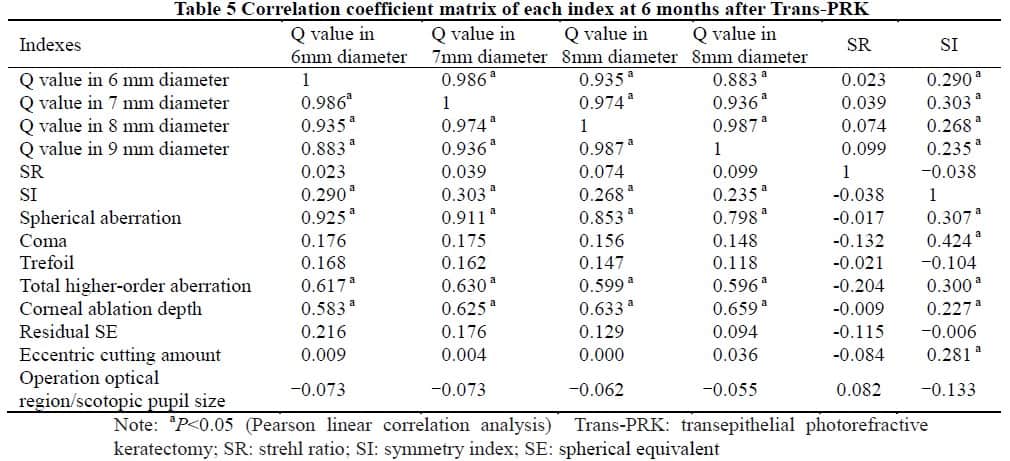
The average preoperative BCVA and SE were -0.09±0.06 and (-4.24±1.24)D.The mean UCVA and SE at 7 days, 1, 3 and 6 months postoperatively were -0.10±0.08 and (0.03±0.63)D, -0.12±0.06 and (0.08±0.53)D, 1.16±0.06 and (0.02±0.79)D, -0.18±0.05 and (0.08±0.37)D, respectively.The SI at different time points after the surgery were significantly higher than that before operation (all at P<0.05). At 1, 3 and 6 months after surgery, the Q value of anterior corneal surface in different diameter ranges increased from negative to positive, showing statistically significant differences (all at P<0.05). At each time point after surgery, the trefoil and total higher-order aberrations of the anterior corneal surface increased to varying degrees.Coma at 7 days and 6 months after surgery were significantly higher than that before surgery, and spherical aberration at 3 and 6 months after surgery were significantly higher than that before surgery (all at P<0.05). The SR values at 3 and 6 months after operation were significantly higher than that before operation (all at P<0.05). At 6 months after operation, the MTF values at different spatial frequencies of the horizontal meridian and the MTF values at 30 and 40c/d spatial frequencies of the vertical meridian were lower than those before operation, and the differences were statistically significant (all at P<0.05). The correlation analysis showed that the Q value of different diameter ranges was positively correlated with spherical aberration (r=0.798-0.925, P<0.05), total higher-order aberration (r=0.596-0.630, P<0.05), SI (r=0.235-0.303, P<0.05) and corneal ablation depth (r=0.583-0.659, P<0.05) at 6 months after surgery.SI was positively correlated with spherical aberration (r=0.307, P<0.05), coma (r=0.424, P<0.05), total higher-order aberration (r=0.300, P<0.05), corneal ablation depth (r=0.227, P<0.05), and eccentric cutting amount (r=0.281, P<0.05). There was no correlation between SR and aberration, corneal ablation depth, eccentric cutting amount, etc.(all at P≥0.05).
Conclusions
Trans-PRK using SPT to correct myopic astigmatism can improve vision, stabilize diopter, enhance retinal imaging quality, increase the asymmetry of the anterior corneal surface, and introduce different degrees of higher-order aberrations.
Key words:
Figures&Tables

Contributor Information
Eye School of Chengdu University of TCM, Ineye Hospital of Chengdu University of TCM, Key Laboratory of Sichuan Province Ophthalmopathy Prevention &
Cure and Visual Function Protection with TCM, Chengdu 610036, China
Eye School of Chengdu University of TCM, Ineye Hospital of Chengdu University of TCM, Key Laboratory of Sichuan Province Ophthalmopathy Prevention &
Cure and Visual Function Protection with TCM, Chengdu 610036, China
Eye School of Chengdu University of TCM, Ineye Hospital of Chengdu University of TCM, Key Laboratory of Sichuan Province Ophthalmopathy Prevention &
Cure and Visual Function Protection with TCM, Chengdu 610036, China
Eye School of Chengdu University of TCM, Ineye Hospital of Chengdu University of TCM, Key Laboratory of Sichuan Province Ophthalmopathy Prevention &
Cure and Visual Function Protection with TCM, Chengdu 610036, China
Eye School of Chengdu University of TCM, Ineye Hospital of Chengdu University of TCM, Key Laboratory of Sichuan Province Ophthalmopathy Prevention &
Cure and Visual Function Protection with TCM, Chengdu 610036, China