Abstract [View PDF] [Read Full Text]
Objective
To compare the clinical effects of minimally invasive vitreous surgery with and without anti-vascular endothelial growth factor (VEGF) drugs for polypoid choroidal vascular disease (PCV) complicated with vitreous hemorrhage.
Methods
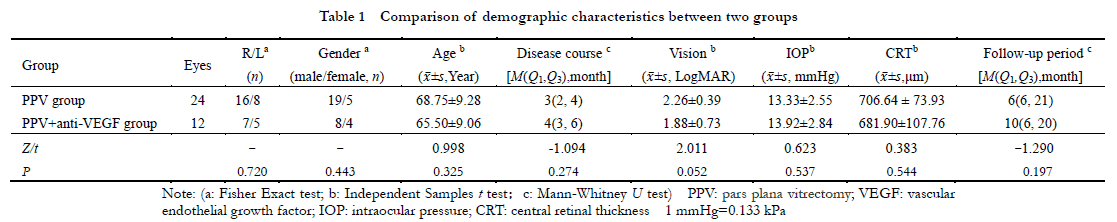
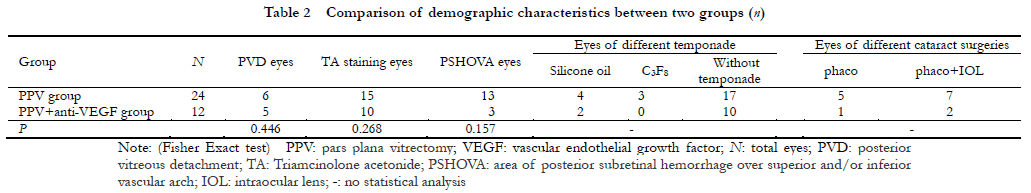
A cohort study was performed.Thirty-six consecutive cases (36 eyes) with PCV combined with vitreous hemorrhage who underwent 25G minimally invasive vitreous surgery in Xuzhou First People’s Hospital from June 2015 to June 2020 were enrolled.According to surgical methods, the patients were divided into pars plana vitrectomy (PPV) group (24 eyes) receiving vitrectomy only and PPV+ anti-VEGF group (12 eyes) receiving vitrectomy first and intravitreal injection of anti-VEGF drugs one week after the operation.All patients were followed up for at least 6 months.The best corrected visual acuity (BCVA) and central retinal thickness (CRT) of the two groups before treatment, 1 month after treatment and at the last follow-up were measured and compared.Postoperative complications such as recurrence of vitreous hemorrhage and macular scar formation were recorded.This study followed the Declaration of Helsinki and was reviewed and approved by the Medical Ethics Committee of Xuzhou First People’s Hospital (No.xyyll[2021]014).Written informed consent was obtained from each patient before surgery.
Results
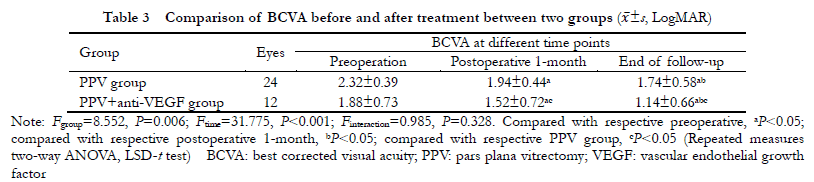
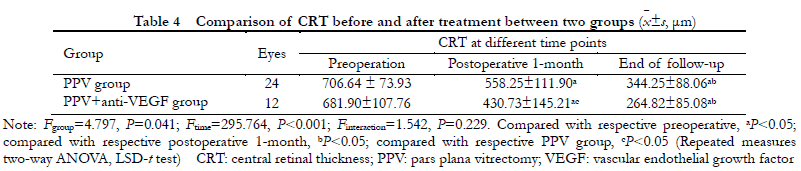
Statistically significant differences were found in BCVA between the two groups before and after treatment (Fgroup=8.552, P=0.006; Ftime=31.775, P<0.001).The BCVA of the two groups at 1 month after operation and at the last follow-up were significantly improved in comparison with before treatment, and the BCVA at the last follow-up was significantly better than that at 1 month after operation (all at P<0.05).One month after operation and at the last follow-up, the BCVA of PPV+ anti-VEGF group was better than that of PPV group, showing statistically significant differences (both at P<0.05).Statistically significant differences were found in CRT between the two groups before and after treatment (Fgroup=4.797, P=0.041; Ftime=295.764, P<0.001).One month after operation and at the last follow-up, the CRT of both groups was significantly improved in comparison with before treatment, and the CRT was significantly better at the last follow-up than 1 month after operation (both at P<0.05).The postoperative 1-month CRT of PPV+ anti-VEGF treatment group was lower than that of PPV group, with statistically significant difference (P<0.05).No statistically significant difference was found in CRT between the two groups at the last follow-up (P>0.05).Elevated intraocular pressure occurred in 2 eyes and rhegmatogenous retinal detachment in 1 eye in PPV group, accounting for 8.33% and 4.17%, respectively.Cataract aggravated in 2 eyes in PPV+ anti-VEGF group.The incidence of vitreous rebleeding in PPV group and PPV+ anti-VEGF group was 16.67%(4/24) and 8.33%(1/12), respectively, with no significant difference (P=0.646).The incidence of macular scarring in PPV group and PPV+ anti-VEGF group was 4.17%(1/24) and 33.3%(4/12), respectively, showing a statistically significant difference (P=0.030).
Conclusions
Minimally invasive vitreous surgery is a safe and effective way to treat PCV combined with vitreous hemorrhage.It can improve vision, reduce CRT, and the effect is gradually enhanced in the short term.Intravitreal injection of anti-VEGF drugs can enhance the postoperative effect of PPV and present better vision and anatomical structure of retina.
Key words:
Figures and Tables
Contributor Information
Department of Ophthalmology, The Affiliated Xuzhou Municipal Hospital of Xuzhou Medical University, Xuzhou First People’s Hospital, Xuzhou Eye Disease Prevention and Treatment Institute, Xuzhou 221116, China
Department of Ophthalmology, The Affiliated Xuzhou Municipal Hospital of Xuzhou Medical University, Xuzhou First People’s Hospital, Xuzhou Eye Disease Prevention and Treatment Institute, Xuzhou 221116, China
Department of Ophthalmology, The Affiliated Xuzhou Municipal Hospital of Xuzhou Medical University, Xuzhou First People’s Hospital, Xuzhou Eye Disease Prevention and Treatment Institute, Xuzhou 221116, China
Department of Ophthalmology, The Affiliated Xuzhou Municipal Hospital of Xuzhou Medical University, Xuzhou First People’s Hospital, Xuzhou Eye Disease Prevention and Treatment Institute, Xuzhou 221116, China
Department of Ophthalmology, The Affiliated Xuzhou Municipal Hospital of Xuzhou Medical University, Xuzhou First People’s Hospital, Xuzhou Eye Disease Prevention and Treatment Institute, Xuzhou 221116, China
Department of Ophthalmology, The Affiliated Xuzhou Municipal Hospital of Xuzhou Medical University, Xuzhou First People’s Hospital, Xuzhou Eye Disease Prevention and Treatment Institute, Xuzhou 221116, China
Department of Ophthalmology, The Affiliated Xuzhou Municipal Hospital of Xuzhou Medical University, Xuzhou First People’s Hospital, Xuzhou Eye Disease Prevention and Treatment Institute, Xuzhou 221116, China