·Clinical Research·
Concordance between Chinese dry eye diagnostic criteria and Asian dry eye diagnostic criteria
Ouyang Weijie1, Liu Zuguo1, Sun Xuguang2, Deng Yingping3, Li Qingsong4, Huang Caihong1, Lin Xiang1, Zhu Li1
1Xiamen University Affiliated Xiamen Eye Center, The Affiliated Xiang’an Hospital of Xiamen University and Eye Institute of Xiamen University, Xiamen 361102, China; 2Beijing Tongren Hospital, Capital Medical University, Beijing 100069, China; 3West China Hospital, Sichuan University, Chengdu 610044, China; 4Putuo District Center Hospital, Shanghai 200062, China
Corresponding author: Liu Zuguo, Email: zuguoliu@xmu.edu.cn
[Abstract] [View PDF in English] [View PDF in Chinese] [Read Full Text]
Objective To analyze the clinical manifestations and signs of the first diagnosed eye patients,and to explore the concordance between the Chinese dry eye diagnostic criteria and the Asian dryevediagnostic criteria.
Methods A cross-sectional multicenter study was conducted. One hundred and forty-one eyes of 141 patients who were diagnosed as dry eye for the first time were included in Xiamen Eye Center of Xiamen University, Beijing Tongren Hospital, West China Hospital of Sichuan University and Shanghai Putuo District Center Hospital from December 2016 to May 2018. All patients completed the Chinese Dry Eye Questionnaire, Ocular Surface Disease Index (OSDI) and Dry Eye-Related Quality-of-life Score Questionnaire (DEQS) to evaluate the symptoms ofdry eye. Tear film breakup time BUT), keratoconjunctival fluorescein staining,meibomian gland morphology and function examination,and Schirmer I test were performed to evaluate dry eye signs and the association between dryeye symptoms and signs. The eyes were divided into corneal staining positive and negative group according to thepresence or absence of corneal fluorescein staining,and the dry eye symptoms of the two groups were assessed by thethree questionnaires. The eyes were divided into tear-deficient dry eye, evaporative dry eye, mixed dry eye and abnormal tear dynamics dry eye to compare the difference of dry eye signs among the groups. This study adhered to the Declaration of Helsinki. The study protocol complied with Chinese regulations and rules on clinical trial research andwas approved by Ethics Committees of Xiamen Eye Center of Xiamen University (No. 2017003), Beijing Tongren Hospital, Capital Medical University No. TREC2016-29), West China Hospital of Sichuan University No. 2016310) and Shanghai Putuo District Center Hospital No.PTEC-A-2016-18-1). Written informed consent was obtained frompatients before entering the cohort.
Results The total score of Chinese Dry Eye Questionnaire,OSDI questionnaire and DEQS questionnaire was 12.00(7.00, 16.00), 25.00(17.50, 36.93) and 32.02(15.77, 52.34), respectively. It was found that 130 eyes (92.2%) had dryness, and 109 eyes (77.3%)had ocular fatigue and 108 eyes (76.6%) had foreign body sensation.Dryness,foreign body sensation,photophobia and poor vision were weakly positively correlated with corneal staining (r=0.177, 0.297, 0.172; all at P<0.05). Pain, photophobia and poor vision were negatively correlated with tear secretion (r=-0.178,-0.197, -0.174; all at P<0.05). It was found that 43.3% of dry eye patients had used visual display terminals. Among the 141 eyes, 75 eyes (53.2%) were with over evaporationdry eye, 43 eyes (30.5%) with mixed dry eye, 18 eyes (12.8%) with aqueous-deficient dry eye and 3 eyes (2.1%) with abnormal tear dynamics dry eyes.
Conclusions Initial diagnosis of dry eye patients is mainly mild tomoderate. Dry eye signs and symptoms are correlated. Over evaporation dry eye is the most common type of dry eye. The concordance between the Chinese dry eye diagnostic criteria and the Asian Dry Eye Society diagnostic criteria reaches 97.2%.
[Key words] Dry eye; Dry eye signs/diagnosis; Dry eye symptoms/diagnosis; Asia Dry Eye Society
DOI: 10.3760/cma.j.cn115989-20211128-00651
Dry eye is a chronic disease of the ocular surface caused by the abnormal quality and quantity of tear fluid induced by multiple factors, causing the stability of the tear film, manifested as dryness, foreign body sensation, tingling sensation, burning sensation, and so forth, affecting the normal work and life of patients, and causing blindness in severe cases1. Dry eye is prevalent in about 30% of the population in China, and the number of patients with dry eye still continues to grow with the aging population and the popularity of video terminal technology. Thorough knowledge of the clinical
characteristics of dry eye is extremely important for understanding its pathogenesis and precise treatment. Despite many clinical studies describing the clinical characteristics of dry eye2-3, the common problem in these studies is that the enrolled patients are not the first clinically diagnosed patients with dry eye; some patients have already received relevant drug treatment, which cannot reflect the essential characteristics of this disease. Reports on the clinical characteristics of patients with dry eye who do not receive medical treatment are lacking. Based on this, the Asian Dry Eye Society conducted a multicenter study on the clinical characteristics of patients diagnosed with dry eye for the first time in China, Japan, and South Korea. The aim was to explore the clinical characteristics of patients with dry eye in Asia, analyze the conformity between dry eye diagnosed according to the diagnostic criteria established by the aforementioned countries and the diagnostic criteria of dry eye in Asia, and provide the basis for the consensus formulation and clinical diagnosis and treatment of dry eye in Asia. This study, with the consent of the Asian Dry Eye Society, reported the results of a multicenter investigation of patients diagnosed with dry eye for the first time in China.
1 Materials and Methods
1.1 Baseline data
A cross-sectional, multicenter study was conducted from December 2016 to May 2018 at the Eye Institute and Affiliated Xiamen Eye Center of Xiamen University, Beijing Tongren Hospital, Sichuan Huaxi Hospital, and Shanghai Puotuo District Center Hospital. A total of 141 patients (44 men and 97 women; the male-to-female ratio: 2:5; mean age: 42.0 ± 14.4 years) diagnosed with dry eye for the first time according to the Chinese expert consensus on dry eye (2013) were enrolled in DECS-C. Among these, 25 patients (17.7%) wore contact lenses, and 61 patients (43.3%) were engaged in video terminal-related workers [visual display terminal (VDT)]; the weekly VDT time was 5-98 h [the average time (48.1 ± 21.4) h]. Furthermore, 14 (9.9%) and 19 patients (13.5%) had other ocular diseases and systemic diseases, respectively. Also, 22 patients (15.6%) were previously treated with nondry eye drugs.
The inclusion criteria were as follows: (1) age ≥ 18 years, (2) sex not limited, and (3) diagnosed with dry eyes for the first time. The exclusion criteria were as follows: (1) those who had received dry eye drugs or dry eye-related treatment; (2) those with a history of fluorescein allergy; and (3) the principal investigator and/or the assisting investigator deeming it inappropriate to participate in the study.
Both eyes were examined by ophthalmologists, and the symptoms were scored using the Chinese Dry Eye Questionnaire; the one eye with high symptom score was used as the study eye. If the scores of both eyes were equal, the heavier eye with corneal fluorescein sodium staining was included. If the degree of sodium fluorescein staining of the cornea of both eyes was comparable, the eyes with a shorter tear film breakup time (BUT) were included. If the BUT was equal, the right eye was considered the study eye. The whole study procedure followed the Declaration of Helsinki and was approved by the Medical Ethics Committee of Xiamen University Affiliated Xiamen Eye Center, Beijing Tongren Hospital, West China Hospital, and Putuo District Center Hospital [2017003, TREC2016-29, 2016(310), PTEC-A-2016-18-1]. Written informed consent was obtained from all the study participants.
1.2 Methods
1.2.1 Quality control The four eye centers standardized and unified the calibration of examination equipment before the project started. The inspectors had Good Clinical Practice (GCP) certificates by Advanced Research Institute of State Drug Administration, including examination items, examination methods, diagnostic criteria, ethics, and so forth. A clinical research coordinator was provided by a third-party company to monitor the quality of the study, track the progress of the study, and coordinate the work of the trial.
1.2.2 Eye examination The patient’s dry eye history was collected, and the clinical examination and laboratory examination were performed. The clinical examination included dry eye questionnaires, BUT, keratoconjunctival staining score, Schirmer I test, and Meibomian gland function score.
1.2.2.1 Dry eye questionnaires The dry eye symptoms were evaluated using the Chinese Dry Eye Questionnaire, Ocular Surface Disease Index (OSDI), and Dry Eye-Related Quality-of-Life Score (DEQS) questionnaire. All patients completed the questionnaires independently under the supervision and guidance of the investigator. The Chinese Dry Eye Questionnaire consisted of 12 questions. Questions 1-6 pertained to evaluating medical history and inducing factors, and questions 7-12 focused on assessing dry eye symptoms. Each question had 0-4 points, totaling 48 points4. The OSDI questionnaire consisted of 12 questions, with each question scoring 0-4 points. According to the calculation formula, the total score was 0-100 points. Patients with dry eye could not only score symptoms using the OSDI questionnaire, but also grade symptoms according to the score. Patients with symptom scores ≤20 were classified as mild dry eye, patients with scores 20 to ≤45 were classified as moderate dry eye, and patients with scores>45 were classified as severe dry eye5. The DEQS questionnaire consisted of 15 questions. Questions 1-6 were aimed at evaluating dry eye symptoms, and questions 7-15 were designed to assess the impact of dry eye on one’s life. The answers were categorized into column A and column B. Column A was the frequency of occurrence, with a score ranging from 0 to 4. Column B was the degree of influence with a score ranging from 1 to 4; column B did not need to be filled in when column A was 0. According to the calculation formula, the total score was 0-100 points6.
1.2.2.2 BUT measurement Tear fluid was stained with fluorescein. Tear film breakup, which exposed the corneal surface, was observed with a slit-lamp microscope. BUT (in seconds) per eye was measured three times, and the mean value was calculated.
1.2.2.3 Determination of corneal staining scores The assessment was made according to the International Institute of Ophthalmology staining scale7. The cornea was categorized into five regions: upper, nasal, middle, lower, and temporal. The score of each region was 0-3 points: 0 indicated no staining, 1 indicated 1-5 staining points, 2 indicated 6-15 staining points, and 3 indicated any of the following: (1) 16 or more staining points; (2) one or more staining sites ≥1 mm in length; and (3) one or more dyeing sites. The total score was the sum of the scores of each cornea area, the highest score was 15, and the total score of ≥1 was abnormal.
1.2.2.4 Determination of keratoconjunctival staining scores The score of fluorescein sodium staining was determined based on the Van Bijsterveld scoring system8. The ocular surface was divided into three regions: temporal conjunctiva, cornea, and nasal conjunctiva. The score of each region was 0–3 points: 0 indicated no injury, 1 indicated visible partial injury, 2 indicated more than half injury, and 3 indicated whole injury. The total score was the sum of the scores of each district. The highest score was 9, and the total score ≥1 was abnormal.
1.2.2.5 Schirmer I test The lacrimal secretion for 5 min was measured in millimeters by inserting a Schirmer test strip with the tip folded into one-third of the outer part of the lower eyelid without an anesthesia under the natural blinking condition. The length of tear infiltration <5 mm was abnormal.
1.2.2.6 Evaluation of Meibomian glands The presence or absence of the following on one-third of the central site of the upper eyelid was confirmed using a slit-lamp microscope.
(1) Abnormal findings around the orifice of Meibomian gland
The presence or absence of the following findings was confirmed.
① Vascular engorgement
② Anterior or posterior replacement of the mucocutaneous junction
③ Irregular lid margin
(2) Orifice obstruction
① Presence or absence of plugging, pouting, and ridge
② Secretion by compression classified as hyper-secretion, normal secretion, and hypo-secretion (obstruction)9
1.2.3 Evaluation target (1) The correlation between ocular symptom score and dry eye-related signs of tested eyes was analyzed. The correlation between dry eye symptom score and physical signs was evaluated. Based on the presence or absence of corneal staining, the tested eyes were categorized into positive and negative corneal staining groups, and the differences in ocular symptom scores between the two groups were compared. (2) The dry eye physical signs were evaluated. (3) The abnormalities and the secretion of Meibomian glands were evaluated. (4) The dry eye symptom score and physical signs in different types of dry eye groups were compared. (5) The diagnosis of dry eye was based on the Asian Dry Eye Association, which included dry eye symptoms plus BUT <5 s10. The coincidence rate between the manifestations of dry eye in the tested eye and the diagnostic criteria of Asian dry eye was assessed.
1.3 Statistical analysis
The calculations were performed using the SPSS Statistics 22.0 software (IBM SPSS, Turkey) and GraphPad Prism version 7 software (CA, USA). The Shapiro-Wilk test was used to perform the normal distribution test for measurement data. The data with normal distribution or near-normal distribution were described by x(_) ± s. The data among groups were confirmed using the Levene test to have homogeneity of variance. The non-normally distributed data were described as M (Q1, Q3). The counting data were described as frequency and percentage. The Kruskal-Wallis H test was used to compare the overall difference in measurement data among different types of dry eye, and the Wilcoxon rank-sum test was used for pairwise comparison between groups. Spearman’s rank correlation analysis was used to evaluate the relationship between Chinese Dry Eye Questionnaire score and OSDI and DEQS scores, and to evaluate the correlation between symptom scores and sign-related indicators of the examined eye. A P value <0.05 indicated a statistically significant difference.
2 Results
2.1 Ocular symptoms of the examined eye and the correlation between symptoms and physical signs of dry eye
2.1.1 Results of Chinese Dry Eye Questionnaire, DEQS questionnaire, and OSDI questionnaire The patients’ overall scores on the Chinese Dry Eye Questionnaire was 12.00 (7.00-16.00), which included 5.00 (2.00-8.00) for medical history and predisposing variables and 6.00 (4.00-9.00) for symptoms of dry eye. Also, 90.8% of the patients experienced dry eyes, making up 128 patients; and 76.6% had ocular foreign body sensation, affecting 108 patients. The overall DEQS score was 32.02 (15.77-52.34), with the dry eye symptom scoring 34.33 (14.58-44.20) and the impact-on-life scoring 30.16 (16.71-48.28). Among the patients, 109 (77.3%) and 130 patients (92.2%) both had eye fatigue. Also, 108 patients, or 76.6%, reported experiencing an ocular foreign body sensation. The individuals had an average OSDI score of 25.00 (17.50-36.93), with scores below 20 points accounting for 50 patients (35.46%), scores between 20 and 45 points for 65 patients (46.10%), and scores above 45 points for 26 patients (18.44%). Further, 107 patients (74.9%) reported feeling an eye foreign body and 98 patients (69.5%) reported experiencing eye pain. OSDI and DEQS scores were favorably correlated with the Chinese Dry Eye Questionnairescore (r = 0.676, 0.679; both P<0.001) (Figure 1).

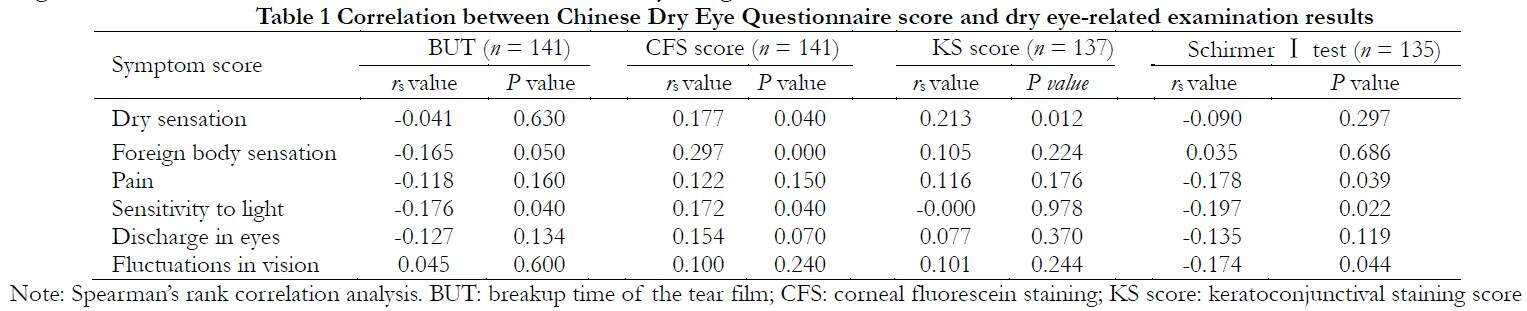
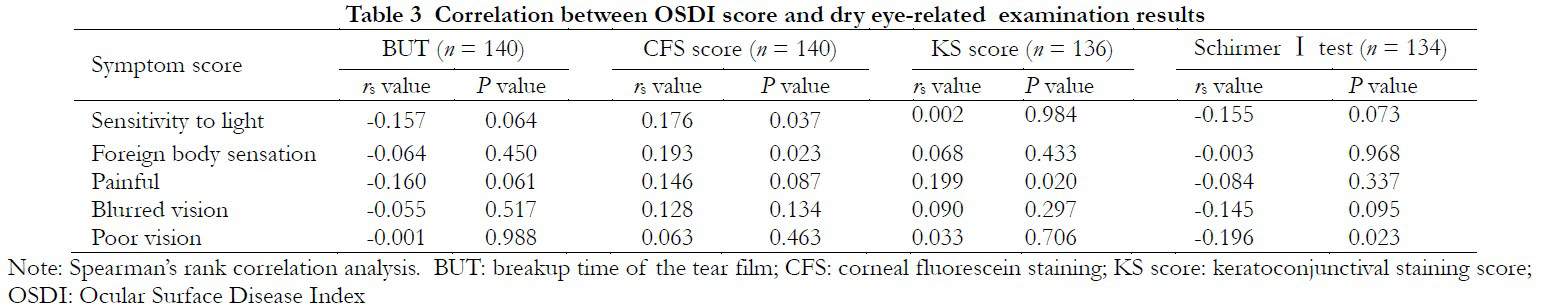
2.1.2 Correlation between ocular symptoms and physical signs of dry eye A weak positive correlation was found between the total score of the Chinese Dry Eye Questionnaire and corneal fluorescein staining scores (rs = 0.312, P = 0.001), and no significant correlation was observed with the results of BUT and Schirmer I tests. A weak negative correlation was noted between BUT and sensitivity to light (rs = -0.176, P = 0.037), and a weak positive correlation was observed between corneal fluorescein staining scores and dry sensation, foreign body sensation, and sensitivity to light (rs = 0.177, P = 0.036; rs = 0.297, P = 0.001; rs = 0.172, P = 0.041). Tear production was negatively correlated with pain, sensitivity to light, and fluctuation in vision (rs = -0.178, P = 0.039; rs = -0.197, P = 0.022; rs = -0.174, P = 0.044). No significant correlation was found between the total score of DEQS questionnaire and dry eye signs (P > 0.05). Corneal fluorescein staining scores had a weak positive correlation with foreign body sensation and heavy sensation in eyelids (rs = 0.255, P = 0.002; rs = 0.204, P = 0.015). BUT and tear production were weakly negatively correlated with the score of heavy sensation in eyelids (rs = -0.272, P = 0.001; rs = -0.249, P = 0.004). No significant correlation was found between the total score of OSDI questionnaire and the dry eye signs (P > 0.05). The corneal fluorescein staining score was weakly positively correlated with sensitivity to light and ocular foreign body sensation (rs = 0.176, P = 0.037; rs = 0.193, P = 0.023). Keratoconjunctival staining scores had a weak positive correlation with ocular pain (rs = 0.199, P = 0.020), and tear production had a weak negative correlation with fluctuations in vision (rs = -0.196, P = 0.023) (Tables 1-3).
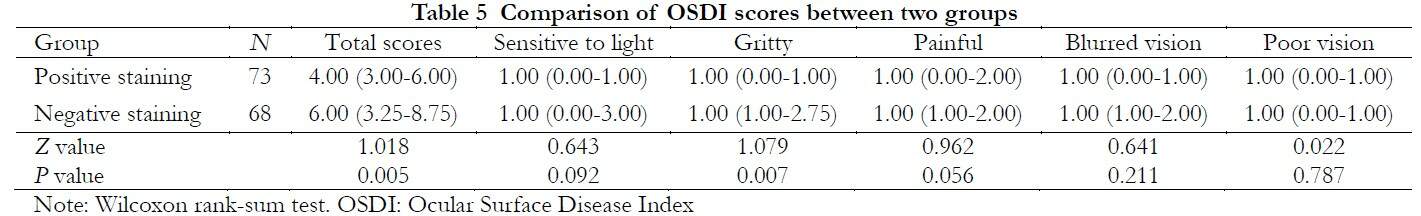
2.1.3 Comparison of questionnaire scores between positive and negative corneal fluorescein staining groups The total symptom score of Chinese Dry Eye Questionnaire was significantly higher in the positive corneal staining group than in the negative corneal staining group, and the difference was statistically significant (P < 0.001). The score of foreign body sensation and discharge in eyes was higher in the positive corneal staining group than in the negative corneal staining group, and the
difference was statistically significant (P < 0.001; P = 0.043). The total score of OSDI symptoms was significantly higher in the positive corneal staining group than in the negative corneal staining group, with statistical significance (P = 0.005). The score of foreign body sensation was higher in the positive corneal staining group than in the negative corneal staining group, with statistical significance (P = 0.007) (Tables 4 and 5).
2.2 Ocular surface physical signs
The average BUT was 3.26 s ± 1.44 s, and 137 patients’ BUT (97.2%) was shorter than 5 s. Schirmer’s I test yielded 10.60 (5.00-13.00) mm/5 min, of which 45 patients (31.9%) were less than 5 mm/5 min. Further, 68 patients (48.2%) had corneal fluorescein staining results that were positive, giving the corneal fluorescein staining score of 1.60 (0.00-2.00).
2.3 Evaluation of Meibomian glands
In evaluating Meibomian gland morphology, 75 patients (53.6%) had marginal hyperemia. Also, 26 patients had Marx’s line shift, accounting for 18.6%; 28 patients (20.0%) had irregular palpebral margins. Further, 85 patients (60.7%) had abnormal Meibomian gland openings. The assessment of Meibomian gland secretion revealed that 11 patients had a high level of secretion, accounting for 7.9%; 66 patients (47.1%) had insufficient secretion.
2.4 Comparison of dry eye symptom score and physical signs in different types of dry eye groups
The four dry eye subgroups: evaporative dry eye (75 patients, 53.2%), mixed dry eye (43 patients, 30.5%), aqueous-deficient dry eye (18 patients, 12.8%), and abnormal tear dynamics dry eye (3 patients, 2.1%) are shown in Table 6.
The results of dry eye signs were different in the subtypes of dry eye. Statistically significant differences were found in BUT, tear production, Chinese Dry Eye Questionnaire score, and OSDI score among evaporative dry eye, mixed dry eye, and aqueous-deficient dry eye (Z = 3.138, 3.678, 10.11, and 8.294; P = 0.047, 0.028, 0.0001, and 0.0004, respectively). Compared with the aqueous-deficient dry eye, the patients in the evaporative dry eye and the mixed dry eye had longer BUT, increased tear secretion, and decreased corneal staining score, and the differences were statistically significant (P < 0.05). The OSDI scores of evaporative dry eye and mixed dry eye were higher than those of aqueous-deficient dry eye, and the differences were statistically significant (P < 0.05). No significant difference in the OSDI score was found between the evaporative dry eye and mixed dry eye (P > 0.05) (Table 6).
2.5 Coincidence rate between the BUT of patients with dry eye and that meeting the diagnostic criteria of Asian dry eye
Among the 141 patients included in this study, 137 patients had BUT less than or equal to 5 s, accounting for 97.2%. That is, about 97.2% of patients with dry eye met the dry eye diagnostic criteria of the Asian Dry Eye Association. Among these, the compliance rate of aqueous-deficient dry eye was 100%, the compliance rate of evaporative dry eye was 97.3%, and the compliance rate of mixed dry eye was 95.3%.
3 Discussion
Most patients included in the traditional dry eye clinical trials received long-term treatment, so they could not reflect the real state of dry eye, leading to researchers’ misunderstanding of dry eye and even improper treatment. This study was novel to include the first diagnosed patients with dry eye as study subject. Compared with patients enrolled in traditional clinical studies, the first diagnosed patients with dry eye did not receive any dry eye-related therapies, excluding confounding factors such as pathophysiological changes in dry eye caused by treatment and ocular surface damage caused by preservatives in eye drops, which could better reflect the pathophysiological state of dry eye and help researchers understand dry eye.
Many previous studies on the correlation between signs and symptoms of dry eye reported inconsistent results3, most of which showed no correlation but some believed a certain correlation2,11-12. Some studies reported that total OSDI score was negatively correlated with tear secretion and positively correlated with corneal staining12, but not correlated with individual symptom and sign13. In this study, the Chinese Dry Eye Questionnaire and total OSDI score were positively correlated with corneal staining score. The correlation analysis of individual symptoms and signs showed that dry eye symptoms were mostly correlated with corneal fluorescein sodium staining and tear secretion volume. The results of this study were different from those of previous studies, which might be because previously enrolled patients had received dry eye treatment before enrollment that affected the patients’ judgment of their own symptoms.
In this study, foreign body sensation was a common symptom in patients with dry eye, and was positively correlated with corneal fluorescein sodium staining score. Further analysis of the symptom scores in patients with positive and negative corneal staining showed that the score of foreign body sensation in patients with negative corneal staining was lower. Also, the score of foreign body sensation increased after the appearance of corneal staining and increased with the aggravation of corneal staining. Although dry eye symptom score was also positively correlated with corneal fluorescein sodium staining score, no significant difference was found in dry eye score between positive and negative corneal staining patients. Similarly, despite differences in the scores of morning secretion (or difficulty in opening eyes) between positive and negative corneal staining patients, no significant correlation was found with the score of corneal fluorescein sodium staining. According to the 2007 International Guidelines for Dry Eye, the severity of corneal fluorescein sodium staining is one of the signs that reflect the severity of dry eye14. Therefore, we believed that the severity of foreign body sensations could reflect the severity of dry eye.
To date, the internationally recognized dry eye questionnaires are OSDI and DEQS, and China has its own dry eye questionnaires, which have their own advantages. The Chinese Dry Eye Questionnaire highlighted that the score of etiology analysis questionnaire was positively correlated with the score of corneal fluorescein sodium staining, which could reflect the correlation between individual symptom and sign. Also, it was mostly correlated with corneal fluorescein sodium staining and tear secretion, but had no significant correlation with BUT. OSDI was used to grade the severity of dry eye symptoms, which could reflect the correlation between single symptom and sign. It was mostly related to corneal fluorescein sodium staining and tear secretion, but had no obvious relationship with BUT. DEQS symptoms included heavy eyelids and redness, and their scores were significantly related to BUT, tear secretion, and corneal fluorescein sodium staining. Besides symptom scores, different questionnaires have different emphases. For example, the Chinese Dry Eye Questionnaire focuses on etiology analysis, whereas OSDI and DEQS questionnaires focus on life quality analysis. Different dry eye questionnaires can be selected based on the main purpose of the study. The Chinese Dry Eye Questionnaire had a significant correlation with OSDI and DEQS questionnaires, but still differences were found among the three. Based on the correlation between symptoms and signs, the correlation between total scores and signs of Chinese Dry Eye Questionnaire and OSDI was higher than that of the DEQS questionnaire, both of which were positively correlated with corneal fluorescein sodium staining scores with a close correlation coefficient. The correlation analysis of individual symptoms and signs showed that the correlation between the score of dry eye common symptoms, such as dry eye and foreign body sensation, in the Chinese Dry Eye Questionnaire and the score of corneal fluorescein sodium staining was better than that of OSDI. The Chinese Dry Eye Questionnaire addresses the living habits of Chinese people, whereas the OSDI questionnaire is designed according to the living habits of foreigners. Therefore, when choosing the OSDI questionnaire, some situations not applicable beyond symptoms may arise. Previously, we found that the accuracy of Chinese Dry Eye Questionnaire was higher than that of OSDI in Chinese patients with dry eye4. Therefore, the Chinese Dry Eye Questionnaire was preferred when selecting dry eye symptom score in China.
At present, no unified standard exists for the diagnosis of dry eye. The instability of tear film is one of the core mechanisms of dry eye, and BUT can reflect the stability of the tear film. In this study, most patients were with mild-to-moderate dry eye, with 97.2% with an average of total BUT less than 5 s, and the results of BUT were more sensitive than those of other tests. In this study, evaporative dry eye accounted for the highest proportion of patients with dry eye, followed by mixed dry eye, aqueous-deficient dry eye, abnormal tear dynamics dry eye, and mucin-deficient dry eye, which was different from the previous finding that the most common type of dry eye in China was mixed dry eye. This might be because the onset time of patients with dry eye in this group was short and the etiology was caused by single or multiple factors. Furthermore, the long-term use of video terminals by VDT workers15, the wearing of contact lenses16, and the increase in environmental factors such as air conditioning environment could promote tear evaporation, leading to the increased incidence of evaporative dry eye. With the progression of dry eye disease, a single type of dry eye eventually develops into mixed dry eye if the treatment is not timely or ineffective. Therefore, mixed dry eye is the most common in the development of dry eye. Lipids secreted by the Meibomian glands constitute the lipid layer of the tear film. Meibomian gland dysfunction (MGD) can cause abnormal secretion of lipids from the Meibomian glands, resulting in fast tear evaporation. Therefore, MGD is the main reason of evaporative dry eye1. In this study, about 60% of the patients had abnormal opening of the Meibomian gland and abnormal palpebral margin, which was similar to the proportion of evaporative dry eyes. This study had no patients with mucin-deficient dry eye, which might be related to the selection of cases. Mucin-deficient dry eye is mainly caused by the damage of epithelial cells of the ocular surface, such as drug-induced dry eye, chemical injury, allergic reaction, and so on. However, such patients were not included in this study. The characteristics observed in this study could not represent the clinical characteristics of patients with these two types of dry eye due to the low proportion of dry eye with abnormal tear dynamics and mucin-deficient dry eye clinically.
The diagnosis of dry eye by the Asian Dry Eye Association includes dry eye symptoms and BUT <5 s, and patients with BUT ≥5 s cannot be diagnosed with dry eye 17. According to the Chinese diagnostic criteria, dry eye can be diagnosed based on one of the following test results: (1) BUT ≤5 s or Schirmer I test ≤5 mm/5 min; and (2) BUT ≤10 s or Schirmer I test ≤10 mm/5 min, accompanied by conjunctival staining. Therefore, those who meet the diagnostic criteria of the Asian Dry Eye Association also meet the Chinese diagnostic criteria for dry eye. In this study, BUT was 5 s to ≤10 s and corneal and conjunctival staining scores were in line with the Chinese diagnostic criteria for dry eye but not with the Asian dry eye diagnostic criteria. Therefore, patients diagnosed with dry eye according to the Chinese diagnostic criteria for dry eye cannot be diagnosed with dry eye according to the Asian diagnostic criteria. In a previous study, patients with dry eye had an average BUT of less than 5 s18. Patients with BUT < 5 s accounted for 94.9% of the total9. These results indicated that BUT was predominantly less than 5 s in patients with dry eye. Most patients with dry eye in China still had short BUT in this study. Therefore, 97.2% of patients who met the Chinese diagnostic criteria for dry eye also met the diagnostic criteria of Asian dry eye.
In conclusion, 97.2% of the patients who met the Chinese diagnostic criteria for dry eye also met the diagnostic criteria for dry eye of the Asian Dry Eye Association. Patients diagnosed with dry eye for the first time were in the mild-to-moderate dry eye stage, and evaporative dry eye was more common. Foreign body sensation was positively correlated with corneal fluorescein staining, which reflected the severity of dry eye. This study was novel to investigate the clinical characteristics of patients diagnosed with dry eye for the first time in China to better reflect the pathophysiological state of dry eye.
This study had some limitations. The small sample size of this study made it impossible to conduct a stratified study on the clinical characteristics of each type of dry eye. Furthermore, this study made classification and diagnosis based on Chinese expert consensus on dry eye published in 2013. Given the new edition of expert consensus on dry eye series, some differences in the diagnosis and classification of patients were included in this study. In this study, 2.8% of patients met the Chinese diagnostic criteria for dry eye but did not meet the Asian dry eye diagnostic criteria. The clinical characteristics of these patients could not be analyzed due to the small number of patients with dry eye. Therefore, large-sample studies are needed to further examine the concordance rate between Chinese and Asian dry eye diagnostic criteria
Acknowledgments We thank Santen Corporation of Japan for providing financial support for this study.
Conflicts of Interest The authors declare no conflicts of interest.
Author Contributions Liu Zuguo, Deng Yingping, and Sun Xuguang participated in the topic selection, research design and standardization, review of data analysis results, revision, and finalization of the intellectual content of this study. Ouyang Weijie was involved in implementing the study, collecting and analyzing experimental data, and writing and modifying the manuscript. Li Qingsong, Huang Caihong, Lin Xiang, and Julie participated in the implementation of the study, parameter measurement, experimental data collection and analysis, and manuscript modification and update.
References
[1] Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II Definition and Classification Report[J]. The Ocular Surface, 2017, 15(3):276-283.
[2] Vitale S, Goodman LA, Reed GF, et al. Comparison of the NEI-VFQ and OSDI questionnaires in patients with Sjogren’s syndrome-related dry eye[J]. Health Qual Life Outcomes, 2004, 2:44.
[3] Bartlett JD, Keith MS, Sudharshan L, et al. Associations between signs and symptoms of dry eye disease: A systematic review[J]. Clin Ophthalmol, 2015, 9:1719-1730.
[4] Zhao H, Liu ZG, Yang WZ, et al. Development and assessment of a dry eye questionnaire applicable to the Chinese population[J]. Chin J Ophthalmol, 2015, 51(9):647-654. DOI: 10.3760/cma.j.issn.0412-4081.2015.09.003.
[5] Ozcura F, Aydin S, Helvaci MR. Ocular surface disease index for the diagnosis of dry eye syndrome[J]. Ocul Immunol Inflamm, 2007, 15(5):389-393.
[6] Sakane Y, Yamaguchi M, Yokoi N, et al. Development and validation of the Dry Eye-Related Quality-of-Life Score questionnaire[J]. JAMA Ophthalmol, 2013, 131(10):1331-1338.
[7] Lemp MA. Report of the National Eye Institute/Industry workshop on Clinical Trials in Dry Eyes[J]. Clao J, 1995, 21(4):221.
[8] van Bijsterveld OP. Diagnostic tests in the Sicca syndrome[J]. Arch Ophthalmol, 1969, 82(1):10-14.
[9] Kawashima M, Yamada M, Suwaki K, et al. A clinic-based survey of clinical characteristics and practice pattern of dry eye in Japan[J]. Adv Ther, 2017, 34(3):732-743.
[10] Tsubota K, Yokoi N, Shimazaki J, et al. New perspectives on dry eye definition and diagnosis: A consensus report by the Asia Dry Eye Society[J]. Ocul Surf, 2017, 15(1):65-76.
[11] Nichols KK, Nichols JJ, Mitchell GL. The lack of association between signs and symptoms in patients with dry eye disease[J]. Cornea, 2004, 23(8):762-770.
[12] Schiffman RM, Christianson MD, Jacobsen G, et al. Reliability and validity of the Ocular Surface Disease Index[J]. Arch Ophthalmol, 2000, 118(5):615-621.
[13] Nichols KK, Nichols JJ, MPH M, et al. The lack of
association between signs and symptoms in patients with dry eye disease[J]. 2004, 23(8):762-770.
[14] Lemp MA, Baudouin C, Baum J, et al. The definition and classification of dry eye disease[J]. 2007, 5(2):75.
[15] Fenga C, Aragona P, Di NC, et al. Comparison of ocular surface disease index and tear osmolarity as markers of ocular surface dysfunction in video terminal display workers[J]. American Journal of Ophthalmology, 2014, 158(1):41-48.
[16] Arita R. Validity of noninvasive meibography systems: Noncontact meibography equipped with a slit-lamp and a mobile pen-shaped meibograph[J]. Cornea, 2013, 32 Suppl 1:S65-70.
[17] Wang H, Liu ZG. Dry eye consensus by Asian Dry Eye Society: interpretation[J]. Chin J Exp Ophthalmol, 2020, 38(10):871-876. DOI: 10.3760/cma.j.cn115989-20200828-00614.
[18] Huang CH, Liu ZG, Li W, et al. Effects of 0.3% sodium hyaluronate ophthalmic solution in the treatment of mild-to-moderate dry eye patients: a multi-center clinical study[J]. Chin J Exp Ophthalmol, 2018, 36(12):936-941. DOI: 10.3760/cma.j.issn.2095-0160.2018.12.008.