Abstract [Download PDF] [Read Full Text]
Objective
To investigate the association of peripheral axial lengths and retinal curvatures with refractive status.
Methods
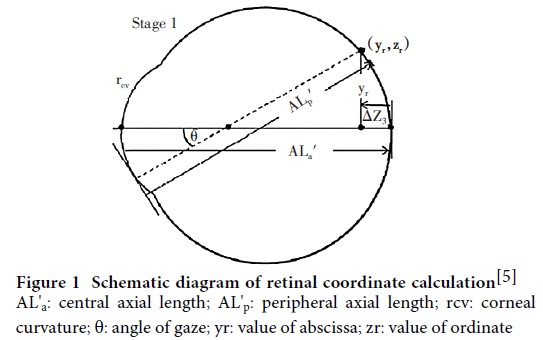
A cross-sectional study was conducted out.Two hundred and eighty-seven eyes of 287 consecutive children aged 6-15 years old who recieved eye examinations at Beijing Tongren Hospital from July to October 2021 were enrolled, including 154 males and 133 females.Uncorrected and best corrected visual acuity were tested with a standard logarithmic visual acuity chart.Spherical equivalent (SE) was measured via an auto refractometer after cycloplegia with tropicamide.The hyperopic, emmetropic and myopic groups were defined with a SE >+ 0.5 D, SE >-0.5 D to ≤+ 0.5 D and SE≤-0.5 D, respectively.Central and 30° peripheral eye lengths (nasal, temporal, superior, inferior) were obtained using the Lenstar LS900.Retinal coordinates were derived from partial coherence interferometry modeling and converted to retinal curvatures.According to the median horizontal peripheral eye length differences (absolute difference between nasal and temporal), participants were assigned to H1 group (absolute difference <0.35 mm) or H2 group (absolute difference ≥0.35 mm). According to the median vertical peripheral eye length differences (absolute difference between superior and inferior), participants were assigned to V1 group (absolute difference <0.32 mm) or V2 group (absolute difference ≥0.32 mm). Four groups of V1H1, V1H2, V2H1 and V2H2 were constructed according to the grouping methods in both directions above.This study adhered to the Declaration of Helsinki.The study protocol was approved by the Ethics Committee of Beijing Tongren Hospital, Capital Medical University (No.TRECKY2021-162). Written informed consent was obtained from guardians of each subject prior to any medical examination.
Results
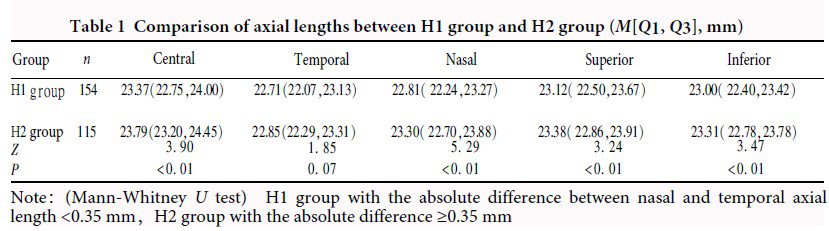
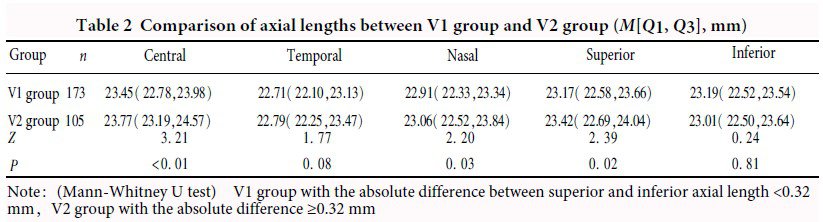
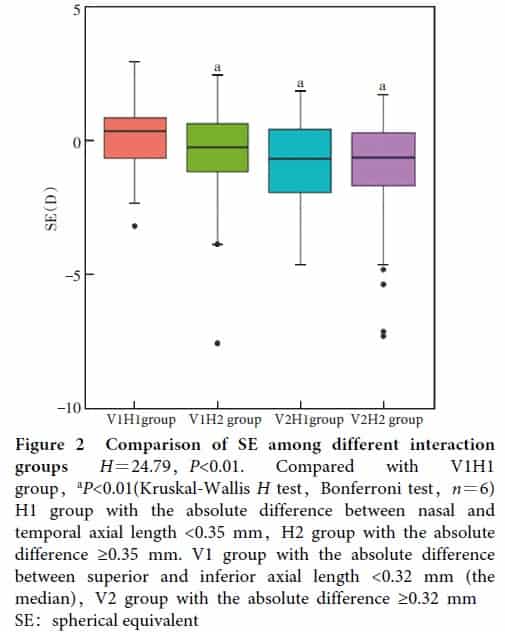
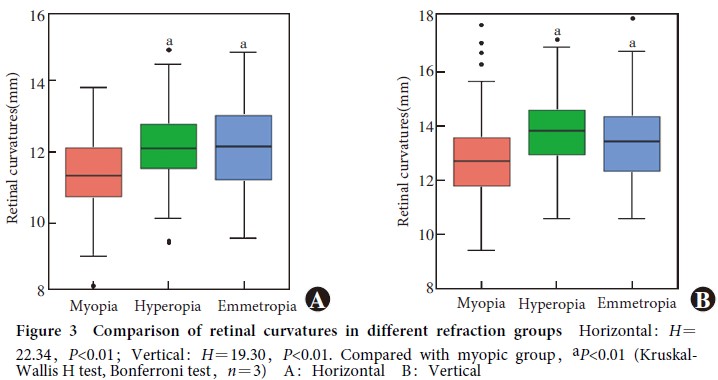
The central axial length was 23.53(22.93, 24.10)mm.Peripheral eye lengths of temporal, nasal, superior and inferior were 22.75(22.11, 23.22)mm, 22.99(22.32, 23.45)mm, 23.24(22.58, 23.75)mm and 23.12(22.52, 23.56)mm, respectively.Temporal eye length was shorter than nasal, showing a statistically significant difference (Z=-3.58, P<0.01). Compared with H2 group, H1 group had shorter central, nasal, superior and inferior eye lengths, showing statistically significant differences (all at P<0.05). Compared with V2 group, V1 group had shorter central, nasal and superior eye lengths, showing statistically significant differences (all at P<0.05). SE of H1 group was + 0.06 (-1.06, + 0.75) D, which was significantly greater than -0.32 (-1.64, + 0.56) D of H2 group (Z=-2.10, P=0.04). SE of V1 group was + 0.13 (-0.81, + 0.80) D, which was significantly greater than -0.56 (-1.83, + 0.48) D of H2 group (Z=-3.39, P<0.01). The myopia ratio of V1 group was 33.5% (58/173), which was significantly lower than 50.5% (53/105) of V2 group (χ2=7.83, P<0.01). There was a significant overall difference in SE among VIH1, V1H2, V2H1 and V2H2 groups (H=24.79, P<0.01). SE was greater in V1H1 group than V1H2, V2H1 and V2H2 groups (all at P<0.01). There was a significant difference in both horizontal and vertical retinal curvatures among different refractive groups (H=22.34, 19.30; both at P<0.01). The retical curvature in both directions of hyperopic and emmetropic groups were significantly larger than those of myopic group (both at P<0.01).
Conclusions
Peripheral eye lengths are asymmetric in school-aged children.Higher asymmetry is associated with myopic shifts.Myopic children have a steeper retina than the hyperopic and emmetropic children.
Key words:
Figures&Tables
Contributor Information
Beijing Tongren Hospital, Tongren Eye Center, Capital Medical University, Beijing Ophthalmology &
Visual Science Key Lab, Beijing 100730, China
Beijing Tongren Hospital, Tongren Eye Center, Capital Medical University, Beijing Ophthalmology &
Visual Science Key Lab, Beijing 100730, China
Beijing Tongren Hospital, Tongren Eye Center, Capital Medical University, Beijing Ophthalmology &
Visual Science Key Lab, Beijing 100730, China
Beijing Tongren Hospital, Tongren Eye Center, Capital Medical University, Beijing Ophthalmology &
Visual Science Key Lab, Beijing 100730, China
Beijing Tongren Hospital, Tongren Eye Center, Capital Medical University, Beijing Ophthalmology &
Visual Science Key Lab, Beijing 100730, China
Beijing Tongren Hospital, Tongren Eye Center, Capital Medical University, Beijing Ophthalmology &
Visual Science Key Lab, Beijing 100730, China
Beijing Tongren Hospital, Tongren Eye Center, Capital Medical University, Beijing Ophthalmology &
Visual Science Key Lab, Beijing 100730, China
Beijing Tongren Hospital, Tongren Eye Center, Capital Medical University, Beijing Ophthalmology &
Visual Science Key Lab, Beijing 100730, China
Beijing Tongren Hospital, Tongren Eye Center, Capital Medical University, Beijing Ophthalmology &
Visual Science Key Lab, Beijing 100730, China
Beijing Tongren Hospital, Tongren Eye Center, Capital Medical University, Beijing Ophthalmology &
Visual Science Key Lab, Beijing 100730, China
Beijing Tongren Hospital, Tongren Eye Center, Capital Medical University, Beijing Ophthalmology &
Visual Science Key Lab, Beijing 100730, China