Authors: Xu Man, Zhang Hongda, Niu Xiaoguang
Wuhan Aier Ophthalmic Hanyang Hospital, 430050
Corresponding author: Niu Xiaoguang, Email: 13476186008@163.com
[Abstract] A 35-year-old female patient with a history of significant epidemiological exposure firstly visited eye doctor due to acute tarsadenitis in the right eye. Subsequently, she developed subconjunctival hemorrhage in the right eye, fever and cough and received topical administration of antibiotics and systemic treatment of antiviral drug. Shortly thereafter, both her mother and father, who denied COVID-19 associated epidemiological history, appeared fever, fatigue and other symptoms and diagnosed as COVID-19. This female patient was diagnosed as COVID-19 by CT image of lung and COVID-19 RNA detection 17 days and 24 days after firstly visited eye doctor, respectively, and received specialized isolation treatment. The symptoms of COVID-19 are very varied, eye doctors should keep alert and pay attention to personal protection.
[Key words] Novel corona virus disease; Tarsadenitis; Subconjunctival hemorrhage; 2019 Novel coronavirus; Prevention and control of epidemic
DOI:10.3760/cma.j.cn.115989-20200228-00121
Since December 2019, an outbreak of 2019 novel coronavirus disease (COVID-19) occurred in Wuhan, Hubei Province, China and spread rapidly worldwide. The pathogenic pathogen was 2019 novel coronavirus (2019-nCoV). The incidence of COVID-19 patients is insidious, highly infectious, and the number of clustered cases increased dramatically. Besides infringing on human respiratory tract, 2019-nCoV also extensively damages other organs and tissues. Its transmission route, prevention and control measures have been the focus of attention after the outbreak, bringing huge challenges to global public health management and medical work. The ocular surface is the exposed tissue and is closely related to the anatomy of the respiratory mucosa. It has been reported that some COVID-19 patients had conjunctivitis as the first symptom or had conjunctivitis during the course of the disease[1-3]. Higher requirements have been put forward for the prevention and control of infection among ophthalmologists. This paper reported the diagnosis and treatment process of a COVID-19 patient, who initially visited eye doctor due to tarsadenitis and subconjunctival hemorrhage.
A 35-year-old female, residents of Wuhan, presented in Wuhan Aier Ophthalmic Hanyang Hospital with complaining of “two-day tenderness in the lateral side of the right eye”. On the evening of January 18, 2020, the patient presented with tenderness and pain in the lateral canthus of the right eye, and lower eyelid swelling without obvious causes. She visited a doctor at a local hospital on January 19 and diagnosed as tarsadenitis of the right eye, and tobramycin dexamethasone eye ointment was topically applied for treatment. One day later, the swelling of the right eye became worse and she was admitted to our hospital. A local inspection showed set of tenderness and pain in the lateral canthus of the right eye accompanying with lower eyelid swelling without known causes. She was diagnosed as right eye acute tarsadenitis by examination, and then tobramycin dexamethasone eye ointment was applied. A routine examination procedure exhibited as Ophthalmic physical including vision: 20/20 in both eyes, IOP 15.0 mmHg for the right eye and 14.3 mmHg for the left eye . The lower eyelid of the right eye was inflamed and a mess in the lateral canthus of the lower eyelid could be palpable with marked tenderness along with palpebral conjunctiva was congestive. The bulbar conjunctiva was normal, the cornea and aqueous humor were clear, and the lens was transparent. The left eye was normal (Figure 1A). A clinical diagnosis was acute tarsadenitis of the right eye. Levofloxacin eye drops was administered once per hour while tobramycin dexamethasone eye drug was applied , and amoxicillin capsule was taken orally.
On January 22, the patient complained that the pain and the swollen of her eye was aggravated accompanied with headache, cough, and elevated body temperature of 38℃. Ophthalmic physical exhibited that theswollen of the lower eyelid in the right eye were limited than before, and the mass was seen in the lateral canthus of the lower eyelid with tenderness (Figure 1B). Blood routine test exhibited that white blood cell (WBC) count was normal; lymphocyte counts (Lym#) and platelet count (PLT) was decreased. We preliminarily excluded the orbital cellulitis caused by acute tarsadenitis. Then the patient history told that, in January 17, she had contacted with relatives on the evening-meal gathering, who were working near Hua Nan (South China Seafood Wholesale) Market in Wuhan. Therefore, the patient was referred to a fever clinics to determine whether it was the infection or not.
On January 23, by an online consultation, the patient expressed a slighter relief of eye pain than before, but the corner of the eye appeared red with her body-temperature of 37.5℃. The mass of the right eye was seen in the lateral canthus of the lower eyelid, hyperemia and swelling limit, bulbar conjunctival hyperemia in the lateral canthus, and patchy subconjunctival hemorrhage (Figure 1C). We instructed the client to continue medication. The patient was not admitted and diagnosed by the fever clinic due to mild symptoms. Oral oseltamivir phosphate capsule and lianhua qingwen capsule were used as prescription.
On January 27, the patient expressed that her temperature returned to normal and the eye-ache eliminate, but still have redness. Ophthalmological examination showed that in the right eye, the mass of the lower eyelid was significantly reduced, however the temporal subconjunctival hemorrhage was observed (Figure 1D). The blood routine examination showed that all the indicators returned to normal. The patient complained that her mother began to have fever and fatigue on January 23rd. While the treatment in the fever clinic, her mother was given blood routine examination, virus nucleic acid test of nasopharyngeal swab, and CT, which was highly suspected of COVID-19. Meanwhile, the father of the patient also developed fever, fatigue and other symptoms on January 27th and then was diagnosed with COVID-19. The patient’s parents had no other history of epidemiological contact.
The patient herself underwent a pulmonary CT examination on February 5, which revealed a small ground-glass opacity under the pleura of the right lower lobe of the lung (Figure 2A), but the virus nucleic acid test of nasopharyngeal swab showed a negative result. The ocular symptoms disappeared. This patient was followed-up to February 11, CT image of the right lower lobe of the lung showed the small ground-glass opacity was slightly reduced (Figure 2B). However, the nucleic acid test results of the second nasopharyngeal swab were still negative. By February 12, the third nucleic acid test of nasopharyngeal swab showed positive, the patient was diagnosed with COVID-19. She was still being treated in isolation at the central resettlement site.
Discussion: As a similarity to the severe acute respiratory syndromes coronavirus (SARS-CoV) and Middle East respiratory syndromes coronavirus (MERS-CoV), 2019-nCoV has enveloped virions with bio-membrane that approximately 50–200 nm in diameter with a single positive-sense RNA genome. The 2019-nCoV has a 79% identity with SARS-CoV and 50% identity with MERS-CoV [4]. The recent study suggests that 2019-nCoV has a similar receptor binding domain structure to SARS-CoV, although amino acid variations occurs in some key residues [5]. Stuctural analysis showed that the 2019-nCoV exhibits a receptor-binding activity with human angiotensin-converting enzyme 2 (ACE2) [5-6] for entering human body and applying its infection. Studies had shown that ACE2 receptor is mainly expressed in renal tubular epithelial cells, intestinal epithelial cells and cardiovascular system, while its expression is relatively low in alveolar epithelial cells, vascular endothelial cells and vascular wall smooth muscle tissues [7-8]. Liu and his colleagues found that ACE2 receptor was expressed in human corneal epithelial cells, corneal endothelial cells, conjunctival epithelial cells and conjunctival capillary endothelial cells as well [9]. Therefore, we hypothesize that 2019-nCoV can transmitted through conjunctiva or cornea in human as well. The infection of many ophthalmologists in the epidemic outbreak in Wuhan has also aroused great attention of ophthalmologists on the prevention of cross infection. During the SARS-CoV epidemic, Loon and Tong had confirmed the presence of viruses in tears [10-11], but no clinical data has been found to show corneal conjunctival infection in SARS-CoV infected patients. At present, clinical researchers in Wuhan found that some COVID-19 patients’ viral nucleic acid of conjunctival sac samples tested positive, and there were also reports of COVID-19 patients with viral conjunctivitis and even conjunctivitis as the first symptom [1-3]. However, the number of these patients is small and there is no specificity of ocular symptoms [12].
In this study, the patient had a clear epidemiological history, and presented the symptoms of acute tarsadenitis before the symptom of fever, local subconjunctival hemorrhage occurred four days later. Acute tarsadenitis is a common characteristics of eyelid disease commonly caused by bacterial infection, and no investigation report links it to virus infection up to date. Theoretically, the acute tarsadenitis with serious local palpebral conjunctival hyperemia and could usually combined with mild bulbar conjunctival hyperemia, While cases of subconjunctival hemorrhage have not been reported. In clinical work and some research reported that some virus infection can cause subconjunctival hemorrhage, such as Coxsackie virus and enterovirus infection [13-14]. Recent studies suggests that the expression of ACE2 was down-regulated after SARS-CoV infection [15], and the downregulation of ACE2 expression may lead to increased vascular permeability [16].
In addition, the patient’s blood routine examination logically showed a significant decrease in the number of platelets besides to the number of lymphocytes in the patient on the day of the onset of fever and then subconjunctive hemorrhage occured. Review the epidemic epidemiological, eye symptoms and COVID – 19 develop process of the patient, we think that the patients who are firstly visiting ophthalmologist because of ocular diseases should be considered as a whole, pay attention to their epidemic history, general disease or even family history, especially during the outbreak of the epidemic. So as to do a good job in the screening and follow-up of epidemic patients, prevention of cross-infection and carefully study the relationship between local symptoms and systemic diseases. In this case, the patient developed monocular disease in the course of diagnosis and treatment. Whether the acute tarsadenitis is related to the decline of immunity caused by the incubation period of systemic viral infection and whether subconjunctival hemorrhage in the patient related to the 2019-nCoV infection has not been determined.
At present, the situation of COVID-19 eye infection is not clear, and the understanding of COVID-19 and 2019-nCoV is still in the process of in-depth research. The diversity of clinical manifestations of COVID-19 and the strong transmission capacity of 2019-nCoV remind clinicians, including ophthalmologists, to take personal protective measures and be on high alert for eye diseases patients first visit in the department during the epidemic.
Reference
[1] Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored[J/OL].The Lancet, 2020[2020-02-26]. https://www.sciencedirect.com/science/ article/ pii/S0140673620303135.DOI:10.1016/S0140-6763(20)3031 3-5.
[2] 叶娅, 宋艳萍, 闫明, 等. 新型冠状病毒肺炎合并结膜炎三例 [J] . 中华实验眼科杂志, 2020, 38 (3): 242-244. DOI: 10.3760/cma.j.issn.2095-0160.2020.0006.
Ye Y, Song YP, Yan M, et al. Novel coronavirus pneumonia combined with conjunctivitis: three cases report[J] .Chin J Exp Ophthalmol, 2020,38(03): 242-244. DOI: 10.3760/cma. j.issn.2095-0160.2020.0006
- 李雪杰, 汪明, 代晶, 等.首发和伴发结膜炎的新型冠状病毒肺炎患者二例报告[J/OL].中
华实验眼科杂志, 2020, 38(2020-03-05)[2020-03-08].http://rs.yiigle.comyufabiao/
1183752.htm. DOI: 10.3760/cma.j.issn.115989-20200303-00133.[网络预发表].
Li XJ, Wang M, Dai J, et al. Novel coronavirus disease with conjunctivitis and conjunctivitis as first symptom: Two cases report [J/OL]. Chin J Exp Ophthalmol, 2020, 38(2020-03-05) [2020-03-08].http://rs.yiigle.comyufabiao/1183752.htm.2020,38:Epub ahead of print.
[4] Xu XT, Chen P, Wang JF, et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for the risk of human transmission[J/OL]. Sci China Life Sci, 2020-01-21[2020-02027]. http://www. doc88.com/p-90099977080932.html. DOI:10.1007/s11427-020-1637-5.
[5] Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding[J/OL]. The Lancet, 2020-01-28[2020-02-27]. https://doi.org/10.1016/S0140-6736(20)302 51-8.
[6] Shi ZL, Zhou P, Yang X, et al. Discovery of a novel coronavirus associated with the recent pneumonia outbreak in humans and its potential bat origin[J/OL]. BioRxiv, 2020-01-22[2020-02-27]. https://www.researchgate.net/publication/338788527_Discovery_of a_ novel_coronavirus_associated_with_the_recent_pneumonia_outbreak_in_humans_ and_its_ potential_bat_origin. DOI:10.1101/ 2020.01.22.914952. 2020.01.23
[7] Hamming I, Timens W, Buhhuis M, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coraunvims. A first step in understanding SARS pathogenesia[J/OL]. J Pathol, 2004,203(2):631-637[2020-02-28]. https://doi.org/ 10.1002/path.1570
[8] Harmer D, Gilbert M, Borman R, et al. Quantitative mRNA expression profiling of ACE2, a novel homolngue of angiotensin converting enzylne[J/OL]. FEBS Lctt, 2002,532(1-2):107-110[2020-02-27]. https://doi.org/10.1016/S0014-5793 (02)03640-2.
[9] 柳林,孙琰,潘欣,等.SARS-CoV S蛋白功能性受体ACE2在人角膜、结膜中的表达[J].中华实验眼科杂志,2004,22(6):561-564.
Liu L, Sun Y, Pan X, et al.Expression of SARS coronavirus S protein functional receptor—Angiotensin-converting enzyme 2 in human cornea and conjunctiva[J]. Chin J Exp Ophthalmol, 2004, 22(6):561-564.
[10] Loon SC, Teoh SC, Oon LL, et al. The severe acute respiratory syndrome coronavirus in tears[J].Br J Ophthalmol, 2004, 88:861-863.
[11] Tong TR, Lam BH, Ng TK, et al. Conjunctivaupper respiratory tract irrigation for early diagnosis of severe acute respiratory syndrome[J]. J Clin Microbiol, 2003,41:5352.
[12] 李雪杰,汪明,陈长征, 等.伴发或首发病毒性结膜炎的新型冠状病毒感染下眼科医师的 防控策略[J]. 中华实验眼科杂志,2020, 38 (3):276-280. DOI: 10.3760/cma.j.issn. 2095-0160.2020.0002.
Li XJ, Wang M, Chen CZ, et al. Ophthalmologists’ stategy for the prevention and control of coronavirus pneumonia with conjunctivitis or with conjunctivitis as the first symptom[J]. Chin J Exp Ophthalmol, 2020, 38 (3):276-280. DOI: 10.3760/cma.j.issn.2095-0160.2020.0002.
[13]Ferrarini A, Milani GP, Bianchetti MG, et al. Acute hemorrhagic edema of infancy associated with Coxsackie virus infection[J]. Arch Pediatr, 2018,25:244.
[14]Lévêque N, Huguet P, Norder H, et al. Enteroviruses responsible for acute hemorrhagic conjunctivitis[J]. Med Mal Infect, 2010,40:212-218.
[15]Kuba K, Imai Y, Rao S, et al. A crucial role of angiotensin converting enzyme 2(ACE2)in SARS coranavirus-induced lung injury[J].Nat Med, 2005,11 (8):875- 879.
[16] Imai Y, Kuba K, Rao S, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure[J]. Nature, 2005,436(7047):112-116.
Figure legends
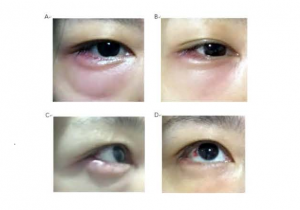
Figure 1. The dynamic development of the acute tarsadenitis A. The second day of acute tarsadenitis, the eyelid of the right eye is inflamed B. The swelling of the lower eyelid lower of the right eye were limited than before C. Bulbar conjunctival hyperemia in the lateral canthus, and patchy subconjunctival hemorrhage D. The mass of the lower eyelid was significantly reduced, and the temporal subconjunctival hemorrhage was observed
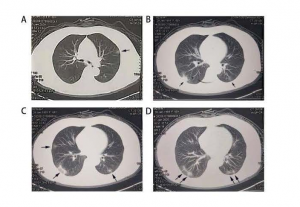
Figuer 2. CT diagnostics of COVID-19 on patient’s mother Panels A, B, C and D showed multiple patchy ground-glass opacity (GGO) in both lungs indicated with arrows in regular four plates of the CT scanning
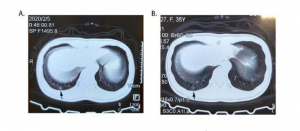
Figuer 3. CT diagnostics of COVID-19 on the patient A: On February 5, the CT showed a small GGO under the pleura of the lower lobe of the right lung with an arrow B. On February 11, the small GGO under the pleura of the lower lobe of the right lung did not change significantly
Table 1. Characteristics on the patient’s routine blood test on January 22
| Inspection Items | Result | Reference Range |
| White Blood Cell | 4.97×10 9 / L | 3.50-9.50(×10 9 / L) |
| Neutrophil Percentage | 78.3% | 40.0%-75.0% |
| Lymphocytes Percentage | 12.7% | 20.0%-50.0% |
| Lymphocyte Count | 0.63×10 9 / L | 1.10-3.20(×10 9 / L) |
| Platelet Count | 73×10 9 / L | 125-350(×10 9 / L) |
Table 2. Characteristics on routine blood test of the patient’s mother on January 27
| Inspection Items | Result | Reference Range |
| White Blood Cell | 4.0×10 9 / L | 3.50-9.50(×10 9 / L) |
| Neutrophil Percentage | 53.3% | 40.0%-75.0% |
| Lymphocytes Percentage | 38.8% | 20.0%-50.0% |
| Lymphocyte Count | 1.6×10 9 / L | 1.10-3.20(×10 9 / L) |
| Platelet Count | 135×10 9 / L | 125-350(×10 9 / L) |
Table 3 Characteristics on common virus test of the patient’s mother on January 27
| Inspection Items | Result | Inspection Items | Result |
| a ADV-IgM | – | f IVA-IgM | – |
| b IVB-IgM | – | g MuV-IgM | – |
| c RSV-IgM | – | h CP-IgM | – |
| d PIVA-IgM | – | i CoxB-IgM | – |
| e MP-IgM | – | j HPVB19- IgM | – |
Note: a: adenovirus; b:influenza virus B; c: respiratory syncytial viral; d: parainfluenza virus; e: mycoplasma pneumonia; f:Influenza virus A; g: mumps virus; h: mhlamydia pneumonia; i:coxsackie virus; j: human parvovirus B19