·Clinical Research·
Multicolor scanning laser imaging in macular telangiectasia
Meng Xiangjuan1, Xie Xiao2, Wang Jinyan1, Sun Xiaolei1, Wang Hongyan1, Meng Jie1, Wang Ying1, Tian Ge1, Guan Jitian1, Zhao Fengyu1, Liu Tingting1
1Eye Hospital of Shandong First Medical University (Shandong Eye Hospital), State Key Laboratory Cultivation Base, Shandong Provincial Key Laboratory of Ophthalmology, Shandong Eye Institute, Shandong First Medical University & Shandong Academy of Medical Sciences, Shandong First Medical University, Jinan 250002, China; 2The First Clinical Medical College, Shandong University of Traditional Chinese Medicine, Jinan 250014, China
Meng Xiangjuan is now working at Cancer Hospital of Shandong First Medical University, Jinan 250117, China
Corresponding author: Liu Tingting, Email:tingtingliu@vip.sina.com
[Abstract] [View PDF in English] [View PDF in Chinese] [Read Full Text]
Objective To observe the characteristics of macular telangiectasia (MacTel) in multi-color and multi-mode fundus images.
Methods A retrospective case series study was conducted. Sixteen eyes of 12 patients diagnosed with MacTel by fluorescein fundus angiography from January to November 2019 in Shandong Eye Hospital were analyzed. There were eight cases (eight eyes) with MacTel type Ⅰ, among which four cases were male and four cases were female, with an average age of 62.3 ± 12.5 years. The other four cases (eight eyes) were MacTel type Ⅱ, all of which were female, with an average age of 58.7 ± 10.5 years. Best-corrected visual acuity, slit lamp microscopy, color fundus photography, colorful fundus laser scanning imaging, fluorescein fundus angiography (FFA), optical coherence tomography (OCT), and optical coherence tomography angiography (OCTA) were conducted for all patients. This study adhered to the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Shandong Eye Institute (No. 2019S003).
Results In color fundus images of MacTel type Ⅰ eyes, annular macular exudation with macular edema occurred in six eyes, macular edema without hard exudation occurred in one eye, and hard macular exudation without macular edema occurred in one eye. However, the transparency of the retinas in temporal fovea in MacTel type Ⅱ eyes decreased, showing a gray color. In multi-color fundus images of MacTel type I eyes, punctate yellow granular macular exudation and yellow-green macular edema were observed, which were clearer than those in color fundus images. Punctate exudation was seen in both the blue reflectance and green reflectance images, which was clearest in green reflectance images, followed by the blue reflectance images, and then infrared reflectance images. In OCT images of MacTel type Ⅰ eyes, cystoid edema of the inner retina or uneven reflection signals of the outer plexiform retina were observed. Loss of inner and outer retinal structures and cavities were observed in MacTel type II eyes, and outer retinal atrophy appeared in two eyes. In OCTA images, the destruction of superficial and deep capillary plexus in the macular area were seen in both MacTel typeⅠand type Ⅱ eyes, with more obvious destruction of the deep capillary plexus. In addition, increased vascular spaces, decreased vessel densities, and
increased foveal avascular zones were found in MacTel type II eyes. In FFA of the early stages, delayed capillary filling near the fovea was seen in MacTel type Ⅰ eyes, and dilated temporal vessels in the fovea, some of which showed tumor-like dilation, and limited tumor-like dilation was enhanced in the later stage. Different degrees of dilated parafoveal blood vessels were seen in the early stage, and the capillary in the temporal side of the macula showed diffuse strong fluorescence in the late stage by FFA in MacTel type Ⅱ eyes.
Conclusions Multi-color fundus laser scanning imaging could be used to show the morphological characteristics of MacTel, indicating that the imaging features of different types of MacTel eyes were significantly different.
[Key words] Retinal telangiectasis; Multimodal imaging; Tomography, optical coherence/angiography; Multi-color image
Funding program: Shandong Key Research and Development Project (2016GSF201088); Shandong Province TCM Science and Technology Development Plan Project (2015-150)
DOI: 10.3760/cma.j.cn115989-20191210-00536
Macular telangiectasia (MacTel) is a disease involving dilation of the parafoveal capillary network in the macula, and neurosensory retinal atrophy, manifesting as visual distortion and progressive visual loss. In earlier studies, the idiopathic parafoveal retinal telangiectasia was defined, which was differentiated from Coat’s disease 1. With ongoing in-depth research, MacTel is divided into three groups, including six subtypes 2. A simplified classification method of idiopathic MacTel was proposed, based on whether MacTel was one of two types, namely, aneurysmal telangiectasia (type I) or parafoveal telangiectasia (type 2) 3. As multiple fundus imaging techniques have been developed in recent years, optical coherence tomography (OCT) and OCT angiography (OCTA) have been widely used in the diagnosis of MacTel 4. Multi-wavelength and multi-color scanning laser fundus imaging can simultaneously scan the superficial, intermediate, and deep retinal structures using three laser beams, and then can acquire the reflection images in different depths and at different layers of tissue structures through superposition and pseudo-color technology 4-6, through which MacTel images can be more intuitively observed. Currently, the analysis of clinical characteristics of multi-wavelength multi-color scanning laser fundus imaging in MacTel has rarely been reported, and the analysis results could provide a basis for the diagnosis and classification of MacTel. Therefore, this study was designed to investigate the characteristics of multi-color scanning laser fundus imaging in different types of MacTel patients.
1 Materials and methods
1.1 General data
A total of 12 patients (16 eyes) diagnosed with MacTel at Shandong Eye Hospital from January to November, 2019 were enrolled and analyzed using case series observations and research methods. The patients enrolled included eight cases (eight eyes) of type I MacTel [four cases (four eyes) of males and four cases (four eyes) of females], with an average age of 62.3 ± 12.5 years, and four cases (eight eyes) of type II MacTel, all of which were females, with an average age of 58.7±10.5 years. All patients complained of reduced vision with or without visual distortions. Intraocular pressure and anterior segment examinations of all eyes revealed no abnormalities. The best-corrected visual acuity (BCVA) of eyes with type I and type II MacTel were 0.05−0.7 and 0.2−0.8, respectively. According to previous studies 3, 7, the inclusion and exclusion criteria were formulated. The inclusion criteria were as follows: 1) patients who were diagnosed as MacTel using fundus fluorescein angiography (FFA) and OCTA, and 2) those with a transparent refractive medium that could ensure a sufficiently clear image. The exclusion criteria involved patients with retinal vascular diseases or other fundus diseases such as inflammation. This study conformed to the Declaration of Helsinki, and the research regimen was approved by the Ethics Committee of Shandong Eye Institute (Approval No.: 2019S003).
1.2 Methods
The BCVA of all patients was examined, and then converted into logarithm of the minimum angle of resolution visual acuity, followed by anterior segment examination using a slit lamp microscope. Subsequently, tropicamide phenylephrine eye drops were used for mydriasis, and then a traditional retinal camera (TRC-50DX; Topcon, Tokyo, Japan) was used for color fundus photography. A Spectralis HRA+OCT (Heidelberg, Germany) was used for FFA, spectral-domain OCT (SD-OCT), OCTA, and multi-color scanning laser fundus imaging.
1.2.1 Color fundus photography
The patients were instructed to sit in front of the retinal camera after full dilation of the pupil. After they looked straight ahead with the head adjusted, color fundus photography was performed, and the obtained photographs were saved.
1.2.2 Multi-color fundus imaging
After mydriasis, in a sitting position, the patients were instructed to place their chin in the chin rest, with the forehead clinging to the rung, and to look at the blue cross cursor in the eyepiece. With the device aiming at the pupil of the patients, the focal length was adjusted until a clear image appeared on the screen. To reduce the strong light exposure time of the patients during the examination, the macular area was initially traced in the infrared (IR) mode, then in the multi-color mode. The examination order was the healthy eye first and then the affected eye.
1.2.3 OCT
The macular area of the patients was traced in the IR mode, and then the structural image of the macular area was obtained in the OCT mode. The image acquisition was performed in a 15°×15° paramacular area using multi-beam (a total of 99 beams with an interval of 120 μm) scanning at a speed of 88,000 times/s.
1.2.4 OCTA
The macular area of the patients was traced in the IR mode, and then subjected to multi-beam (a total of 384 beams with an interval of 11 μm) scanning in the OCTA mode. The images were acquired in a 15°×15° paramacular area at a speed of 68,000 times/s. Later, the blood flow in the macular area was observed.
1.2.5 FFA
The patients initially underwent an allergy test to sodium fluorescein, and those with a negative skin test quickly received an injection of 3 mL of 20% sodium fluorescein in the median elbow vein of the forearm within 5 s. At the beginning of the injection, the angiography time was recorded. The whole FFA procedure required 15 min.
Imaging of the same patient was completed by the same physician on the same day. If the scanning position and image quality did not meet the requirements, or there were excessive pseudo-motions, the imaging was repeated, and the retinal structure was manually segmented, if necessary. Two professionally trained ophthalmologists were responsible for the diagnosis, image reading, and quality review of images. If the imaging reading results obtained by the two ophthalmologists were not the same, a consensus was reached by participation of a third ophthalmologist based on his/her review of imaging reading results.
2 Results
2.1 Color fundus images of MacTel eyes
As shown in the color fundus images of type I MacTel eyes, lipid exudation with yellow pigment showing an unclear margin and the macular edema with an obscure boundary occurred in six eyes, macular edema without hard macular exudation occurred in one eye, and hard macular exudation without edema occurred in one eye. In addition, the color fundus images of type II MacTel eyes showed that the macula, especially the temporal side of the macula, was grey because its transparency was decreased in eight eyes, and tiny crystalline deposits were found in some areas (Figure 1).

2.2 Characteristics of multi-color scanning laser fundus imaging
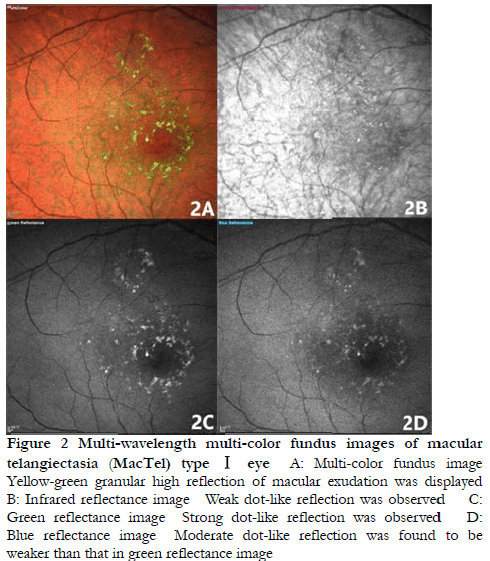
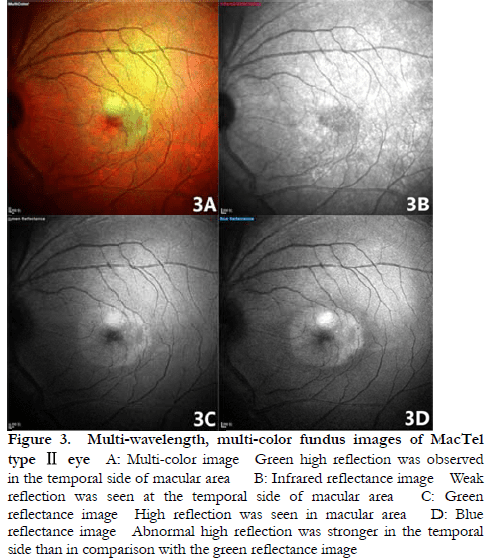
As revealed by multi-color fundus images of type I MacTel eyes, macular edema with green pigmentation was present, and yellow-green granular reflection of exudation was observed, with a clear boundary. Stronger granular reflection was observed in the green reflectance image than blue reflectance image, and the weakest granular reflection was observed in the IR reflectance image (Figure 2). Type II MacTel eyes showed high green reflection in the macula, especially in the temporal side of the macula. The strongest dot-like reflection was found in the blue reflectance image, followed by the green reflectance image and the IR reflectance image (Figure 3).
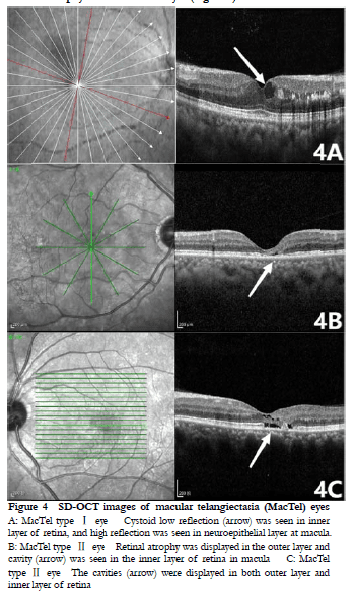
2.3 Characteristics of MacTel SD-OCT
In SD-OCT images of type I MacTel eyes, cystoid edema of the inner retina, and uneven high reflection signals of the outer plexiform layer of retina were observed in six eyes, punctate high reflection in the outer plexiform layer of the macular region in one eye, and only macular edema in one eye. Moreover, in SD-OCT images of type II MacTel eyes, partial defects in the inner and outer structures of the retina and formation of retinal cavities were seen in three eyes, and losses of the outer structure of the retina and macular atrophy were seen in five eyes (Figure 4).
2.4 Characteristics of MacTel OCTA
As displayed in OCTA images of MacTel eyes, destruction of the superficial and deep capillary plexus in the macular area, especially deep capillary plexus destruction, was detected in type I MacTel eyes, which led to tumor-like dilation of parafoveal annular capillaries. Additionally, diffuse dilation of capillaries in the temporal side of the macula, destruction of the superficial and deep capillary plexus in the macular area, increased vascular space, decreased vessel density, and expanded foveal avascular zone were observed in type II MacTel eyes, with variations in the deep capillary plexus being more remarkable (Figure 5).

In the early stage, type I MacTel eyes had delayed filling of the parafoveal capillaries and dilated temporal vessels, some of which showed tumor-like dilation, and the limited tumor-like dilation was enhanced in the late stage (Figure 6). However, type II MacTel eyes showed different degrees of parafoveal small blood vessel dilation of the macula in the early stage, and diffuse strong fluorescence in the temporal capillaries of the macula in the late stage (Figure 6).
2.5 Characteristics of MacTel FFAFigure 5 OCTA images of macular telangiectasia (MacTel) eyes The superficial and deep capillary plexus in MacTel Ⅰ eyes showed destruction and tumor-like dilatation (arrow). Destruction of capillary plexus, increased gaps between blood vessels, and significantly decreased vessel densities (arrow) were observed in the superficial and the deep capillary plexus in MacTel Ⅱ eyes, with changes more obvious in the deep capillary plexus

3 Discussion
According to the evaluation of fundus images in population studies, the prevalence of MacTel is 0.022−0.1% 8. However, the tactual prevalence may be underestimated because of diagnosis using only color fundus photography, so multi-color scanning laser fundus imaging and multi-mode imaging contribute to a better early diagnosis because of its clear and accurate images. In this study, in the color fundus images of type I MacTel eyes, macular edema with or without exudation was observed. The multi-color scanning laser fundus images of type I MacTel eyes displayed green macular edema and yellow-green granular high reflection of exudation. For type II MacTel eyes, color fundus images showed decreased macular retinal transparency, displayed in grey color, especially in the temporal side, and fine crystalline deposits were visible in some areas. In addition, multi-color fundus images showed clear green high reflection in the temporal side of the macula.
Furthermore, green reflection in multi-wavelength, multi-color scanning laser fundus images mainly reflected the inner layer of the retina, including the inner and outer plexiform layers and inner nuclear layer. Blue reflection mainly represented the surface of the retina and the contact tissue between the vitreous and the retina 6. In this study, the green and blue reflection images of MacTel eyes displayed positive manifestations, showing characteristic high reflection of the parafovea. In comparison with common color fundus photography, multi-color scanning laser fundus imaging can show the morphological changes of the macular surface more intuitively and clearly, thus greatly reducing the possibility of misdiagnosis and missed diagnosis.
In this study, SD-OCT images of type I MacTel eyes showed a strong reflection signal of the cystoid edema in the inner retina and/or uneven reflection signals in the outer plexiform layer of the retina. This abnormal reflection was consistent with that shown in multi-color fundus photography. As displayed in OCTA images of type I MacTel eyes, destruction of the superficial and deep capillary plexus in the macular area, especially the deep capillary plexus destruction, was detected, which led to tumor-like dilation of parafoveal annular capillaries. FFA images showed that in the early stage, type I MacTel eyes showed delayed filling of the parafoveal capillaries and dilated temporal vessels, some of which showed tumor-like dilation, and the limited tumor-like dilation was enhanced in the late stage. This result was consistent with the description of previous studies 9. Type II MacTel is characterized by changes in the macular capillary network and exhibits neuroepithelial atrophy in both eyes. In the early stage, the type II MacTel lesion is confined to the temporal side of the macula, and in the later stage, it develops in the parafovea 8-11. In the present study, SD-OCT images of type II MacTel eyes showed losses of inner and outer structures of the retina, and the formation of retinal cavities, and atrophy of the retinal inner layer was seen in two eyes, which was consistent with the results of research conducted by Spaide 12. There was no cystoid macular edema in the affected eyes, which was consistent with the results found by Charbel Issa et al. 13 that type II MacTel eyes generally did not have cystoid macular edema. Additionally, destruction of the superficial and deep capillary plexus in the macular area, increased vascular spaces, and decreased vessel densities were found using OCTA images, the blood vessels in the macular area were stretched to the temporal side, and the temporal blood vessels in the macular area were distorted and dilated.
The exact pathological mechanism of MacTel remains elusive. Some studies have shown that type I telangiectasia is a result of the functional or structural destruction of the blood-retinal barrier, which leads to damage of the blood vessel wall, aneurysm formation, or telangiectasia 8. There are slight, patchy non-perfusion areas or capillary ischemia and lipid deposition in the fundus of the affected eye. Lipids are mostly associated with abnormal capillaries, or persistent, focal, and larger aneurysms 3. In this study, the multi-color scanning laser fundus images showed that the retinal surface showed granular yellow-green reflections, and stronger granular reflections were observed in green reflectance images than in the blue reflectance images and IR reflectance images, which was consistent with the pathological characteristics of lipid exudation in the outer plexiform layer.
Regarding type II MacTel eyes, Powner et al. 14-15 conducted a histopathological study on two type II MacTel eyes, and found that Müller cells and photoreceptors were lost in the affected eyes, suggesting that Müller cell dysfunction was the early and possible pathological feature of type II MacTel eyes. According to a report by Spaide 12, the vitreoretinal traction force on the temporal side of the macula is crucial for the traction of the tissues in the paramacular area and the formation of the right-angle transposition vein. In this study, the strongest reflection was found in blue reflectance images, followed by green reflectance images and IR reflectance images, which suggested that pathological changes on the vitreoretinal surface occurred in type II MacTel eyes.
In summary, studies of multi-mode fundus images were helpful in understanding MacTel at a deeper level and from multiple aspects, and provided more options for its early diagnosis and differential diagnosis. Multi-wavelength, multi-color scanning laser fundus imaging was an effective tool for MacTel examination. In contrast to traditional color fundus photography, it could display the lesions in more depth and more effectively, facilitating early screening and observation of changes in paramacular telangiectasia. There were still some limitations in this study, such as the small sample size, which needs to be further expanded for verification in the future. The clinical features of MacTel largely differed in different types, which suggested that the vitreoretinal interface and retinal blood vessels may have exerted different effects in the pathogenesis of different MacTel types, which should be further validated in the future.
Conflict of Interest All authors declare that there is no conflict of interest.
Author Contributions Liu, TT and Meng, XJ designed the study, and drafted and revised the manuscript; Xie, X produced pictures and revised the manuscript; Wang, JY and Sun, XL conducted clinical examination and image reviews; Wang, HY and Meng, J conducted clinical examinations; Wang, Y managed patients; and Tian, G, Guan, JT, and Zhao, FY collected data and performed literature retrieval.
References
[1] Gass JD. A fluorescein angiographic study of macular dysfunction secondary to retinal vascular disease. V. Retinal telangiectasis[J]. Arch Ophthalmol, 1968, 80(5):592-605. DOI: 10.1001/archopht.1968.00980050594005.
[2] Chew E, Gillies M, Bird A. Macular telangiectasia: a simplified classification[J]. Arch Ophthalmol, 2006, 124(4):573-574. DOI: 10.1001/archopht.124.4.573.
[3] Yannuzzi LA, Bardal AM, Freund KB, et al. Idiopathic macular telangiectasia. 2006[J]. Retina, 2012, 32 Suppl 1:450-460. DOI: 10.1097/iae.0b013e31823f9a59.
[4] Yang JY, Chen YX. Application of optical coherence tomography angiography for diagnosis in fundus diseases[J]. Chin J Exp Ophthalmol, 2017, 35(10):944-948. DOI: 10.3760/cma.j.issn.2095-0160.2017.10.020.
[5] Ben Moussa N, Georges A, Capuano V, et al. MultiColor imaging in the evaluation of geographic atrophy due to age-related macular degeneration[J]. Br J Ophthalmol, 2015, 99(6):842-847. DOI: 10.1136/bjophthalmol-2014-305643.
[6] Pang CE, Freund KB. Ghost maculopathy: an artifact on near-infrared reflectance and multicolor imaging masquerading as chorioretinal pathology[J]. Am J Ophthalmol, 2014, 158(1):171-178. DOI: 10.1016/j.ajo.2014.03.003.
[7] Engelbert M, Yannuzzi LA. Idiopathic macular telangiectasia type 2: the progressive vasculopathy[J]. Eur J Ophthalmol, 2013, 23(1):1-6. DOI: 10.5301/ejo.5000163.
[8] Aung KZ, Wickremasinghe SS, Makeyeva G, et al. The prevalence estimates of macular telangiectasia type 2: the Melbourne Collaborative Cohort Study[J]. Retina, 2010, 30(3):473-478. DOI: 10.1097/IAE.0b013e3181bd2c71.
[9] Chen YG, Chang YH. Multimodal imaging in the diagnosis of macular telangiectasia type 1[J/OL]. Asia Pac J Ophthalmol (Phila), 2022(2022-02-07)[2022-07-26]. http://www. ncbi.nlm.nih.gov/pubmed/35131996. DOI: 10.1097/APO.0000000000000476.[published online ahead of print]
[10] Shinkai A, Saito W, Hashimoto Y, et al. Morphological features of macular telangiectasia type 2 in Japanese patients[J]. Graefe’s Arch Clin Exp Ophthalmol, 2021, 259(5):1179-1189. DOI: 10.1007/s00417-020-04989-x.
[11] Pauleikhoff L, Heeren T, Gliem M, et al. Fundus autofluorescence imaging in macular telangiectasia type 2: MacTel Study Report Number 9[J]. Am J Ophthalmol, 2021, 228:27-34. DOI: 10.1016/j.ajo.2021.03.022.
[12] Spaide RF. Volume-rendered angiographic and structural optical coherence tomography[J]. Retina, 2015, 35(11):2181-2187. DOI: 10.1097/IAE.0000000000000764.
[13] Charbel Issa P, Gillies MC, Chew EY, et al. Macular telangiectasia type 2[J]. Prog Retin Eye Res, 2013, 34:49-77. DOI: 10.1016/j.preteyeres.2012.11.002.
[14] Powner MB, Gillies MC, Tretiach M, et al. Perifoveal Müller cell depletion in a case of macular telangiectasia type 2[J]. Ophthalmology, 2010, 117(12):2407-2416. DOI: 10.1016/j.ophtha.2010.04.001.
[15] Powner MB, Gillies MC, Zhu M, et al. Loss of Müller’s cells and photoreceptors in macular telangiectasia type 2[J]. Ophthalmology, 2013, 120(11):2344-2352. DOI: 10.1016/j.ophtha.2013.04.013.