Recovery of retinal structural damage after repeated low-intensity red light therapy for high myopia: a case report
Tian Yu, Xiao Zhigang
Department of Ophthalmology, Hunan Provincial Children’s Hospital, Changsha 410016, China
Corresponding author: Tian Yu, Email: 2733324706@qq.com
DOI: 10.3760/cma.j.cn115989-20221119-00539
【Download PDF in English】【Download PDF in Chinese】 【Read Full Text】
The patient, a 12-year-old girl, has had myopia for 4 years. After wearing orthokeratology lenses, she repeatedly experienced symptoms such as red eyes, itching, and increased secretions for a year. She sought treatment at Hunan Children’s Hospital on March 12, 2022. Due to a history of allergic conjunctivitis, she had used olopatadine eye drops and hyaluronic acid eye drops for both eyes. Her mother has moderate myopia, but there’s no history of other eye diseases in the family. For the patient’s right eye, the uncorrected visual acuity is 0.04. After pupil dilation with compound tropicamide eye drops, the corrected visual acuity is -6.50 DS/-0.50 DC× 5° =0.8. For her left eye, the uncorrected visual acuity is 0.04, and the corrected visual acuity is -5.75 DS/-1.00 DC× 180° =0.8. Given the patient’s previous use of orthokeratology lenses for myopia correction and repeated episodes of bilateral conjunctivitis, and after ruling out macular diseases through a fundus examination (Figure 1) as requested by her guardian, she was treated using a red light therapy device (model RS-200) employing the repeated low-level red-light (RLRL) method. The instrument is a Class II, Type B device. The light source output power is (2.0± 0.5) mW. With a pupil diameter of 4.0 mm, the light power entering the pupil is approximately 0.25 mW. The irradiation parameters are AC (220± 22) V, (50± 1) Hz; and the input power is ≤ 30 VA. The patient underwent irradiation twice daily for both eyes, with at least a 4-hour interval between sessions, each session lasting 3 minutes. After one month of RLRL treatment, the refractive power of both eyes decreased by approximately -2.00 D, leading to a change in lenses. After three months of treatment, the corrected visual acuity was 1.0. Fundus examinations and optical coherence tomography (OCT) scans were conducted one and three months post-treatment, respectively, and no abnormalities were detected (Figures 2 & 3). Five months post-treatment, on August 10, 2022, the patient experienced rainbow-like afterimages following the treatment, occasionally lasting for over 8 minutes. She didn’t seek medical attention and continued the treatment on her own. On August 30, 2022, she experienced a decline in vision. After consultation, it was advised to discontinue RLRL and to revisit the doctor promptly.
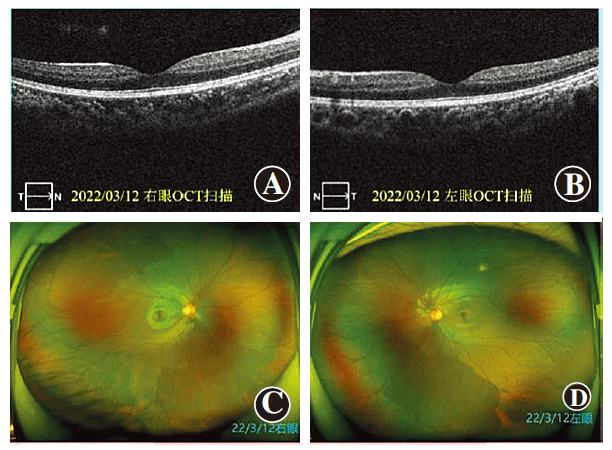
Figure 1 Images of both eyes’ fundus and OCT before RLRL treatment The examination of both eyes’ fundus and OCT did not show any significant abnormalities A: OCT of the right eye B: OCT of the left eye C: Color photograph of the right eye fundus D: Color photograph of the left eye fundus
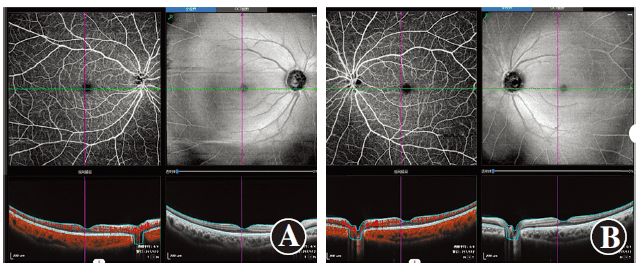
Figure 2 Images of both eyes’ fundus and OCT one month after RLRL treatment The examination of both eyes’ fundus and OCT did not show any significant abnormalities A: Right eye B: Left eye
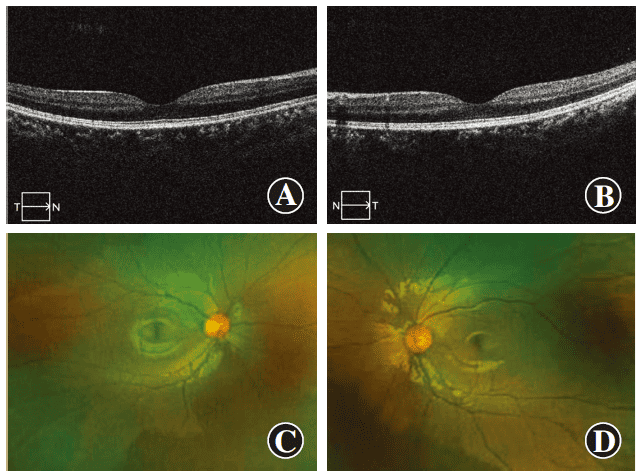
Figure 3 Images of both eyes’ fundus and OCT three months after RLRL treatment The examination of both eyes’ fundus and OCT did not show any significant abnormalities A: OCT of the right eye B: OCT of the left eye C: Color photograph of the right eye fundus D: Color photograph of the left eye fundus
On September 3, 2022, she went to the Hunan Children’s Hospital, complaining of redness in the right eye, photophobia accompanied by coughing and a runny nose for a week, without any fever. An ophthalmological examination revealed conjunctival hyperemia in both eyes, and a patchy fluorescein sodium staining was observed in the central cornea of the right eye. Both eyes exhibited inadequate accommodation and relaxation. Ultra-wide-angle fundus imaging revealed a round lesion at the macular fovea. OCT scans showed discontinuity in the ellipsoid zone of the outer retinal layer at the fovea of both eyes, with a diameter of 712 μm (Figure 4). After a joint consultation with the Refraction Department and the Fundus Diseases Department, the diagnosis was bilateral high myopia, right eye keratitis, left eye conjunctivitis, and retinal changes in both eyes. The patient was prescribed Xeljanz (tofacitinib) medical gel and hyaluronic acid eye drops, to be used for 2 weeks. She was also prescribed oral methylprednisolone, 8 mg/day, to be taken in the morning continuously for 1 week; and a periocular injection of triamcinolone acetonide injection, 40 mg, administered once.
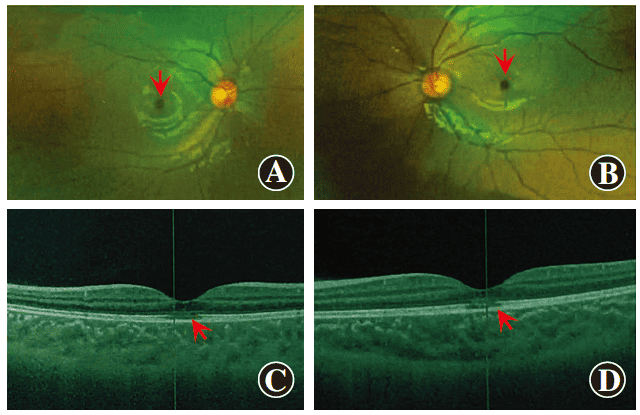
Figure 4 Images of both eyes’ laser scanning confocal ultra-widefield fundus and OCT five months after RLRL treatment Both eyes show a circular lesion in the macular fovea (indicated by arrows in images A and B) and a discontinuity in the outer retinal ellipsoid zone of the fovea (indicated by arrows in images C and D) A: Ultra-widefield fundus image of the right eye B: Ultra-widefield fundus image of the left eye C: OCT of the right eye D: OCT of the left eye
Subsequently, the patient visited Xiangya Second Hospital of Central South University, Xinhua Hospital affiliated with Shanghai Jiao Tong University, and Zhongshan Ophthalmic Center of Sun Yat-Sen University for further examination. An MRI of the optic nerve, both plain and contrast-enhanced, showed no abnormalities in the bilateral optic nerves, but there were significant abnormalities in the visual fields of both eyes. The multifocal electroretinogram (mfERG) showed a reduction in the amplitude density of the first ring in both eyes, with the disappearance of the central response peak. Both eyes had a slight reduction in the amplitudes of both rod and cone response waves. The patient was advised to take oral lutein for 1 month and to discontinue RLRL. Two months later, the patient felt her vision gradually improving. On October 19, 2022, she revisited Hunan Children’s Hospital, where the corrected visual acuity of both eyes had recovered to 0.8. OCT imaging showed that the integrity and continuity of the ellipsoid zone in the macular fovea of both eyes had been restored (Figure 5). She was prescribed hyaluronic acid eye drops and levodopa tablets at 250 mg/day orally. On December 21, 2022, (four months after discontinuing RLRL), her cornea appeared clear, the retinal structure was intact, but the visual acuity of both eyes was not examined (Figure 6).
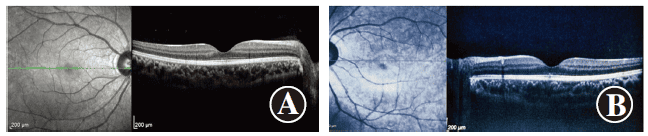
Figure 5 Images of both eyes’ OCT two months after discontinuing RLRL Both eyes show a noticeable improvement in the continuity of the ellipsoid zone in the macular fovea A: Right eye B: Left eye
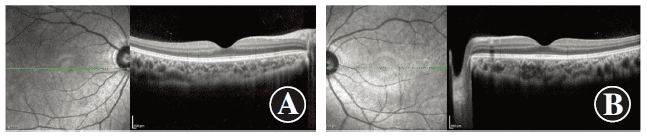
Figure 6 Images of both eyes’ OCT four months after discontinuing RLRL Both eyes show a restored integrity of the retinal structure A: Right eye B: Left eye
3 Discussion
RLRL is a myopia prevention and control method developed in recent years. Its effective control rate on myopia diopter and axial progression over 6-24 months has been confirmed by 7 randomized controlled clinical trials [1-9] and 2 non-randomized controlled studies [10-11]. In March 2022, China’s Ministry of Education and 14 other departments issued the “2021 Comprehensive Myopia Prevention and Control for Children and Adolescents Implementation by the Ministry of Education and Fifteen Other Departments”, emphasizing the need to strengthen scientific research on myopia prevention and control and support multi-center clinical research on myopia prevention and treatment in children and adolescents, such as clinical trials on red light control of myopia.
To standardize the application method of RLRL treatment and control of myopia and monitor its safety, experts in myopia prevention and control and retinal diseases formed a research group. They jointly developed the “Expert Consensus on Repeated Low-Intensity Red Light Irradiation for Assisting in the Treatment of Myopia in Children and Adolescents (2022)” [12]. This consensus emphasized that if after-images occur during the treatment process, they should be closely monitored, especially if the after-image lasts for more than 6 minutes. If the irradiated eye repeatedly presents prolonged after-images, the duration of the after-image should be recorded, and a retinal function and structure examination should be performed under the guidance of a professional doctor. It’s necessary to fine-tune the irradiation frequency or dose and evaluate the measures to stop the irradiation. In the currently published studies on the adverse events of RLRL in controlling myopia, no visual function or retinal structural damage related to RLRL has been found [1-11]. However, due to the strict standards for inclusion criteria and research protocols in randomized controlled studies, the application of RLRL in real-world clinical practice still faces some unresolved scientific issues, and its safety is of great concern.
RLRL involves irradiating the retina with a 650nm red light emitted by a semiconductor diode laser. The actual power measured through a 4mm pupil diameter is 0.29 mW, which is much lower than the national standard of China (GB7247.1-2012), the standards of the US Food and Drug Administration (FDA), and the International Electrotechnical Commission (IEC), which specify 0.40mW. This places it in the Class I category of lasers, which pose no injury risk to the human eye [13-14]. To our knowledge, this is the first reported case of reduced best corrected visual acuity accompanied by retinal structural damage after the widespread clinical research of RLRL. In this case, a 12-year-old child with high myopia switched to the RLRL method due to discomfort from orthokeratology lenses. Shortly after irradiation, the refractive error decreased by about 2.00D. Despite experiencing prolonged afterimages, the child continued RLRL treatment to maintain myopic control, resulting in decreased visual function and structural damage to the retina. This usage does not comply with the safety requirements of the “Expert Consensus on Repeated Low-Intensity Red Light Irradiation to Assist in the Treatment of Myopia in Children and Adolescents (2022)”. The cornea and lens only absorb short-wavelength light, and long-wavelength red light is not absorbed by the cornea. Therefore, it is speculated that although the child’s decreased visual acuity in the right eye was accompanied by symptoms of keratitis and respiratory infections, keratitis is not a potential complication of RLRL treatment. Moreover, the child’s myopic degree decreased by 2.00D just one month into the treatment, suggesting a strong sensitivity to light exposure. This indicates that individualized treatment plans should be considered or that treatment duration should be reduced.
Photoreceptor cells in the macular region are rich in rhodopsin and are the most sensitive to light-induced damage. After treatment, the OCT examination of the patient in this case revealed discontinuity in the ellipsoid zone of the macular fovea and chunky reductions, which is similar to macular damage caused by laser pens [13-14]. Laser pens with a power exceeding 5.0mW can cause damage to the myoid zone, ellipsoid zone, interdigitation zone, and outer nuclear layer of the macula, and even lead to macular holes. According to literature reports, early manifestations of macular damage caused by high-energy laser pens include highly reflective particles or clumps at the central fovea of the macula, which may be accompanied by high reflection in the outer nuclear layer, serous exudation, and retinal pigment epithelial detachment. Over time, these highly reflective particles or clumps gradually decrease or disappear. However, the rupture of the ellipsoid zone and the interdigitation zone is irreversible [14]. After the adverse reaction occurred in this case, communication with the product manufacturer revealed that the treatment instrument has had the function of monitoring output power from the backend since 2019. The equipment used for this patient did not detect any abnormalities in the backend monitoring, and this has been verified by authoritative departments.
Currently, there is a lack of consensus and high-level evidence-based medical evidence for the treatment of retinal photodamage. Common methods include oral corticosteroids and neurotrophic and circulatory improvement therapies [15-16]. Hossein et al. [17] reported a case of retinal damage caused by a laser in a 25-year-old male. The retinal structure was restored within one week after oral corticosteroids. Liang et al. [15] reported a 29-year-old male patient with a macular hole caused by blue laser (light source 450nm, power 150 mW). After taking lutein, multivitamins, and ginkgo biloba leaves orally, the macular structure was restored in 4 weeks, and vision improved from 0.5 to 1.0. Turaka et al. [18] reported a 13-year-old patient with a right-eye laser injury. One day after the injury without treatment, the vision improved from 0.2 to 0.3 on its own, but the damage to the outer layer of the macula remained unchanged. Weng et al. [19] reported a case of a 12-year-old child with retinal damage caused by a laser pen (100 mW). The initial vision was 20/60. OCT examination showed ruptures in the myoid zone, ellipsoid zone, and outer membrane. Four weeks later, the vision improved to 20/25, accompanied by a restoration of the continuity of the outer membrane. However, all the above literature are case reports, and it is difficult to determine whether the improvement in structure and function is spontaneous or due to the effect of drugs. In this case, based on previous retinal damage treatment protocols, oral corticosteroids and triamcinolone acetonide injections were used, and visual function and structure gradually recovered. However, the risk-benefit ratio of corticosteroids and trace elements for children urgently needs clarification.
The severity of photoretinal injury is related to the photo-thermal effects, mechanical damage, and photochemical effects caused by the irradiation power and duration [20]. The wavelength of the light source is also related to safety. The safety of 633-650nm red-orange light is better than 400-500nm green-blue light [16,18]. Although some cases may experience irreversible vision decline and visual field defects, most patients can see improvements in vision and structure, and those with minor injuries can fully recover [13,21]. Since the power of RLRL is approximately 20 times lower than the power threshold that causes retinal damage by laser pens, even if the extremely rare photoretinal injury occurs, the damage to the macular structure and function is reversible. In this case, the ellipsoid zone and interdigitation zone of the child’s retina did not completely rupture, and the retinal structure and function gradually recovered after discontinuing RLRL.
In the prevention and control of myopia in children and adolescents, vision decline combined with retinal structural damage caused by RLRL ocular irradiation is very rare. This case involved retinal structure and function damage in the child. After timely cessation of irradiation and medical intervention, the child’s vision recovered, reminding us that in clinical practice, we should monitor the RLRL ocular irradiation process, timely manage it based on the patient’s tolerance, and adhere to the safety requirements of the “Expert Consensus on Repeated Low-Intensity Red Light Irradiation to Assist in the Treatment of Myopia in Children and Adolescents (2022)”.
Conflict of Interest: All authors declare that there is no conflict of interest.
References (omitted)