·Clinical Research·
Repeatability of CASIA2 for measuring the tilt and decentration of crystalline lens and intraocular lens under non-mydriatic and mydriatic conditions
Tang Yuling, Liao Xuan, Tan Qingqing, Qian Jiulin, Yang Li, Zhou Guimei, Lan Changjun
Department of Ophthalmology, Affiliated Hospital of North Sichuan Medical College, Medical School of Ophthalmology & Optometry, North Sichuan Medical College, Nanchong 637000, China
Corresponding author: Lan Changjun, Email: lanchangjun@sina.com
Abstract [View PDF in English] [View PDF in Chinese] [Read Full Text]
Objective To investigate the repeatability and correlation in tilt and decentration measurement of crystalline lens and intraocular lens (IOL) under non-mydriatic and mydriatic conditions using swept-source ocular coherence tomography CASIA2.
Methods A diagnostic test study was conducted. A total of 109 cataract patients (157 eyes) who received phacoemulsification with IOL implantation surgery in the Affiliated Hospital of North Sichuan Medical College from March to July 2020 were enrolled. The decentration and tilt of crystalline lens and IOL under non-mydriatic and mydriatic conditions were measured for three times by a single examiner using CASIA2 before and one week after surgery. The 0.5% compound tropicamide eye drops were used to dilate. Repeatability was evaluated by within-standard deviation, test-retest repeatability (TRT), coefficient of variation (CoV) and intraclass correlation coefficient (ICC). The correlation in decentration and tilt of crystalline lens and IOL between before and after mydriasis was assessed by Pearson correlation coefficient. This study adhered to the Declaration of Helsinki, and the study protocol was approved by an Ethics Committee of the Affiliated Hospital of North Sichuan Medical College (No. 2020ER030-1). Written informed consent was obtained from all subjects before any medical examination.
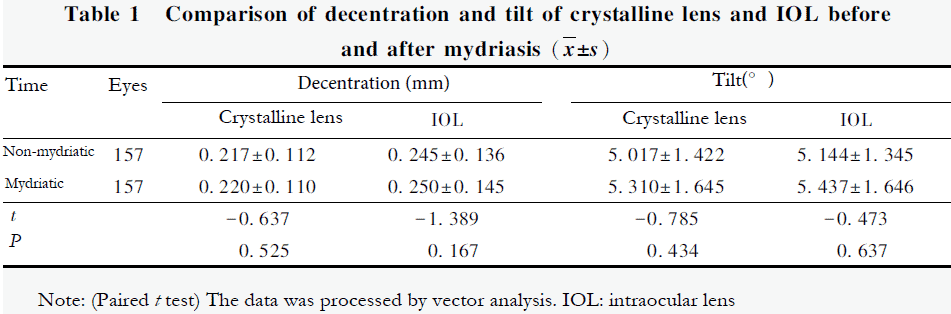
Results The decentration of crystalline lens under non-mydriatic and mydriatic conditions was (0.217±0.112) mm and (0.220±0.110) mm, respectively, and the tilt was (5.017±1.422) ° and (5.310 ± 1.645) °, respectively. The decentration of IOL under non-mydriatic and mydriatic conditions was (0.245±0.136) mm and (0.250±0.145) mm, respectively, and the tilt was (5.144±1.345)° and (5.437±1.646)°, respectively. No significant difference was found between non-mydriatic and mydriatic conditions (all at P>0.05). Under both non-mydriatic and mydriatic conditions, the crystalline lenses of both eyes decentered and tilted toward the inferotemporal direction, and the IOL of right eyes decentered toward the inferior and tilted toward the inferotemporal direction, and the IOL of left eyes decentered and tilted toward the inferotemporal direction. Except the crystalline lens decentration, the measurement repeatability of crystalline lens tilt, IOL decentration and tilt in cataract patients before and after mydriasis was good, with ICC range in 0.815-0.984, TRT<50% and CoV 14.840%. The measurement repeatability of crystalline lens decentration was poor, and the measurement repeatability of decentration axis, tilt and tilt axis of crystalline lens, and the repeatability of decentration and tilt of IOL were good in both eyes, with ICC range in 0.757-0.998, TRT<50% and CoV≤ 17.763%. There were good correlations in decentration, decentration axis, tilt and tilt axis of crystalline lens and IOL between non-mydriatic and mydriatic conditions (all r≥0.679, all at P<0.01).
Conclusions The measurement repeatability of decentration axis, tilt and tilt axis of crystalline lens and IOL, as well as the decentration of IOL by CASIA2 before and after mydriasis is good. The correlations of the measured parameters before and after mydriasis are good.
Key words Tomography, optical coherence/swept-source; Diagnostic test; Cataract; Lenses, intraocular; Decentration; Tilt; Repeatability
Fund program: Key Project of Sichuan Health and Family Planning Commission (18ZD022); Key Project of Nanchong City and University Cooperation (18SXHZ0492)
DOI: 10.3760/cma.j.cnll5989-20210526-00323
With the rising popularity of refractive cataract surgery, the positioning of the intraocular lens (IOL) after cataract surgery is receiving increasing attention. The IOL should be implanted in the capsular bag with the center aligning with the visual axis. However, the patient, the IOL, and the surgical procedure have been known to effect IOL decentration and tilt. This is known to cause high-order aberrations, particularly coma aberrations, deterioration of postoperative visual quality, visual disturbances (e.g., glare), refractive error, and a decrease in visual acuity.1-4 Unpredictable astigmatisms were more sensitive to decentration and tilt after toric IOL implantation.5 Considering these complications, accurate measurement of decentration and tilt in crystalline lens and IOL is extremely important. Previously the pupillary axis, a central line perpendicular to the anterior corneal surface that passes through the center of the pupil, was a commonly utilized reference for assessing IOL decentration and tilt,6-8 but is dependent on pupil size and shape.9 Corneal topographic axis (СТА) is not affected by pupil size and thus serves as a better reference for assessing the IOL decentration and tilt.10 The CASIA2 has been developed as a novel anterior segment swept-source optical coherence tomography (SS-ОСТ) device that measures IOL decentration and tilt using CTA. This study investigates the repeatability of decentration and tilt measurements of the crystalline lens and IOL in Chinese cataract patients using CASIA2. Differences in decentration and tilt of the crystalline lens and IOL before and after mydriasis were also compared to assess the feasibility of clinical measurement under non-mydriatic conditions.
1 Materials and Methods
1.1 General information
This was a diagnostic test study. The sample size was calculated using the following formula: .11 A minimum of 96 eyes were required. Patients were consecutively recruited from Department of Ophthalmology, Affiliated Hospital of North Sichuan Medical College from March to July 2020. A total of 157 eyes (right eyes=80, left eyes=77) of 109 cataract patients underwent phacoemulsification with IOL implantation were enrolled. Of these, 44 were male (44%) with a mean age of 69.85 ± 9.14 years (range, 48-88). Mean axial length (AL) measured by IOLMaster 700 was 23.65 ± 0.86 mm with a range of 21.67 to 26.37 mm. Patient inclusion criteria were as follows: 1) diagnosed with cataract and voluntarily accepted the relevant examinations of this trial; 2) normal tear film function; 3) pupil diameter 3 mm; 4) normal cognitive ability and can be followed up on time. Patients with the following conditions were excluded: 1) ocular disease or neuropathy that may cause vision loss, such as ocular trauma, lens luxation, pseudoexfoliation syndrome, glaucoma or fundus lesions; 2) intraoperative or postoperative complications, such as posterior capsular rupture, incomplete capsulotomy following continuous circular capsulorhexis, or severe posterior capsular opacity; 3) previous intraocular surgery; 4) AL <20 mm or >27 mm; 5) postoperative intraocular pressure (IOP) >21 mmHg (1 mmHg=0.133 kPa); 6) crystalline lens opacity affecting the tilt and decentration measurements; 7) poor understanding and inability to cooperate. This study was conducted in accordance with the Declaration of Helsinki. The protocol was approved by the Ethics Committee of the Affiliated Hospital of North Sichuan Medical College (NO. 2020ER030-1). Written informed consent was obtained from all patients before participating.
1.2.2 Methods
1.2.1 Surgical techniques All surgeries were performed by a single experienced ophthalmologist in accordance with the same protocol. Each patient received a 2.4 mm corneal incision at 10:30 o’clock position and injected with viscoelastic substances under local anesthesia. A continuous circular capsulorrhexis with a diameter of 5.5-5.8 mm was performed. Following phacoemulsification and cortical cleanup, viscoelastic substances were injected into the cartridge. An IOL (SN60WF, Alcon, USA) was implanted into the center of the capsule bag, with its haptics placed at 3 and 9 o’clock position, respectively. Then, viscoelastic substances were removed. After forming of the anterior chamber, the corneal incision was watertight. Tobramycin dexamethasone eye ointment was applied to the conjunctival sac after the surgery.
1.2.2 Decentration and tilt of crystalline lens and IOL examined by CASIA2 For all patients decentration and tilt of the crystalline lens and IOL were evaluated using CASIA2 (Tomey, Japan), and were performed by the same technician before and one week after cataract surgery. The crystalline lens and IOL were measured using the Pre-op Cataract and Post-op Cataract modes on the CASIA2 device. Following 5 minutes of relaxing their eyes, patients were instructed to stare at the fixation lamp to capture the images. The magnitudes and axes of decentration and tilt were calculated with respect to the CTA. Mydriasis was induced by 0.5% tropicamide (Santen, Japan). Three repeated measurements were conducted before and after mydriasis.
1.3 Statistical Analysis
All statistical analyses were performed using SPSS 26.0 statistical software. The Kolmogorov-Smirnov test confirmed a normal distribution, and variables were expressed as means and standard deviations (SDs). The decentration and tilt of the crystalline lens and IOL before and after mydriasis were compared with the paired t test. Repeatability was evaluated by within-standard deviation (Sw), test-retest repeatability (TRT), coefficient of variation (CoV), and intraclass correlation coefficient (ICC). Sw was calculated based on one-way ANOVA.12 The lower the Sw value, the better the repeatability. TRT, or 2.77 Sw, denotes that there is a 95% probability that the absolute difference between the two repeated measurements is less than or equal to this value.13 TRT has a maximum limitation of 50%, and the lower the TRT value, the better the repeatability.14 The CoV is the ratio of Sw to mean, and the lower the CoV value, the better the repeatability. The ICC is one of the indicators to evaluate the confidence. High, moderate, and poor consistency are considered as ICC≥0.90, 0.75<ICC<0.90, and ICC≤0.75, respectively.15 The correlation in decentration and tilt of the crystalline lens and IOL between before and after mydriasis was assessed by Pearson correlation coefficient. Means of three repeated measurements of the decentration and tilt were calculated by vector analysis, as described by Holladay et al.16 A P value less than 0.05 was considered statistically significant.
2 Results
2.1 Comparison of the decentration and tilt of crystalline lens and IOL before and after mydriasis
There were no significant differences in the crystalline lens and IOL decentration and tilt measured by CASIA2 before and after mydriasis (all P at>0.05; Table 1).
 2.2 Repeatability of CASIA2 in the decentration and tilt measurement of crystalline lens and IOL before and after mydriasis in cataract patients
2.2 Repeatability of CASIA2 in the decentration and tilt measurement of crystalline lens and IOL before and after mydriasis in cataract patients
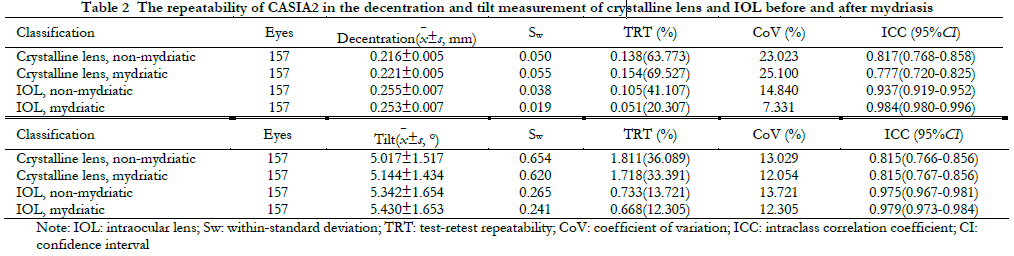
Regarding the crystalline lens decentration measured by CASIA2, the ICC was 0.817 and 0.777 under non-mydriatic and mydriatic conditions, respectively. The respective figures for CoV were 23.023% and 25.100%. TRTs were greater than 50% under both conditions. The repeatability of crystalline lens decentration measurement was poor. Regarding the crystalline lens tilt, IOL decentration and tilt, the repeatability was high (ICC ranged 0.815-0.984. TRTs<50%, CoV ranged 7.33-14.84%; Table 2).
 2.3 Repeatability of CASIA2 in the decentration and tilt measurement of crystalline lens and IOL before and after mydriasis in both eyes
2.3 Repeatability of CASIA2 in the decentration and tilt measurement of crystalline lens and IOL before and after mydriasis in both eyes
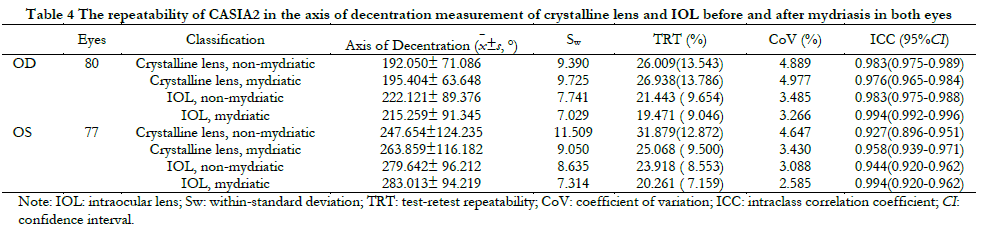
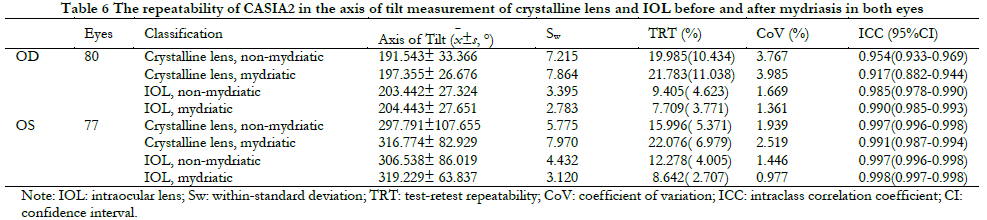
The repeatability of binocular crystalline lens decentration measurement before and after mydriasis was poor (ICC ranged 0.737-0.856, TRT>50%, CoV ranged 20.06-26.82%). The measurements of the axis of decentration of crystalline lens, the magnitude and axis of tilt of crystalline lens, and IOL decentration and tilt in both eyes before and after mydriasis were repeatable (ICC ranged 0.757-0.998, TRT<50%, CoV ranged 0.98-17.76%; Table 3-6).


2.4 Distribution of the decentration and tilt of crystalline lens and IOL before and after mydriasis among cataract patients
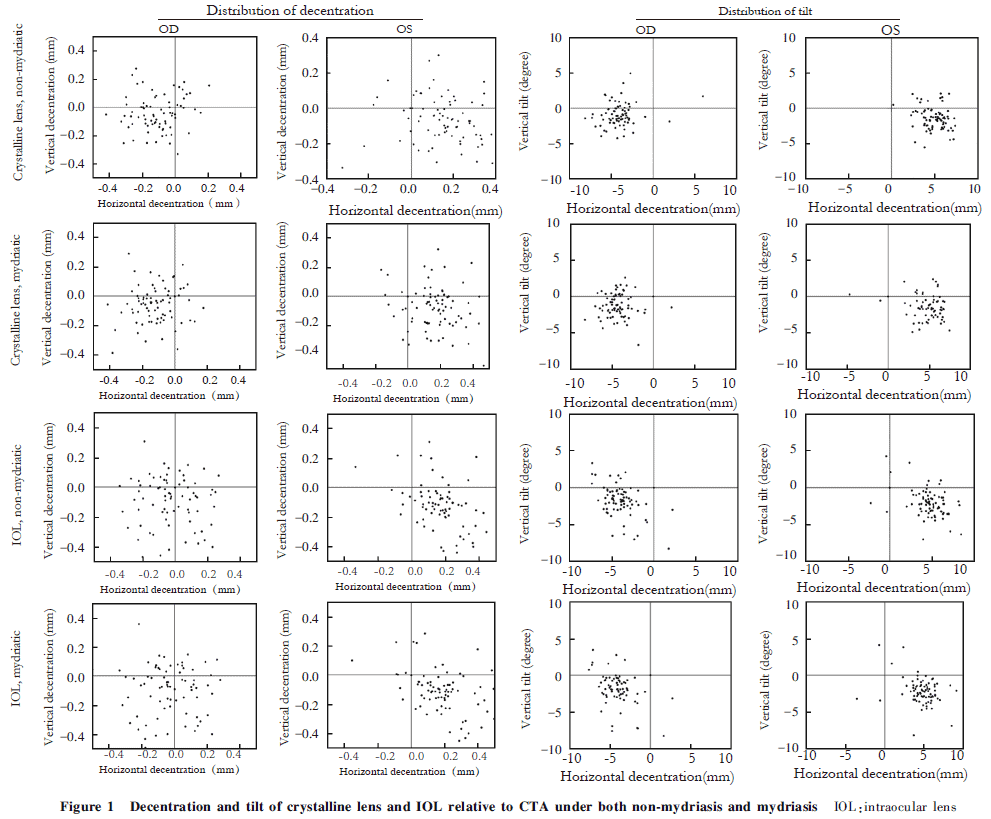
Under non-mydriatic and mydriatic conditions, right and left crystalline lenses were decentered and tilted inferotemporally in a symmetric manner. The IOLs of the right and left eyes were decentered to inferior and inferotemporal directions, respectively. IOL of both eyes tilted inferotemporally in a symmetric manner (Figure 1).
2.5 Correlation of the decentration and tilt of crystalline lens and IOL measured by CASIA2 before and after mydriasis
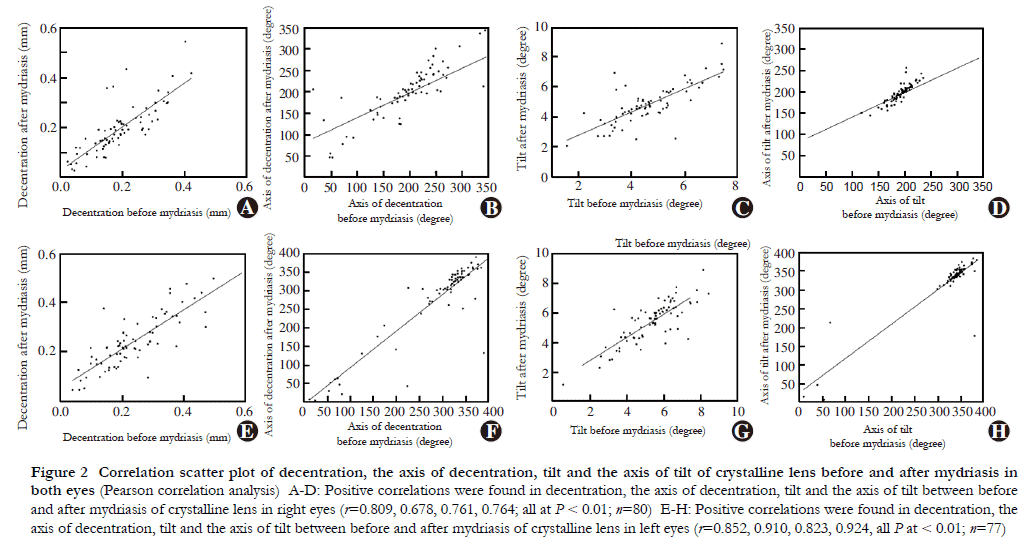
Magnitude of crystalline lens decentration and tilt, and axis of crystalline lens decentration and tilt correlated significantly and positively before and after mydriasis (right eyes: r=0.809, 0.761, 0.678 & 0.764, respectively, all P<0.01; left eyes: r=0.852, 0.823, 0.910, &0.924, respectively, all P<0.01). Magnitude of IOL decentration and tilt and axis of IOL decentration and tilt also correlated significantly and positively before and after mydriasis (right eyes: r=0.941, 0.966, 0.824 & 0.956, respectively, all P<0.01; left eyes: r=0.964, 0.944, 0.972 & 0.995, respectively, all P<0.01; Figures 2 & 3).

3 DiscussionWith the increasing popularity of functional IOLs and emphasis on postoperative visual quality, positioning of the implanted lens is becoming increasingly important for cataract surgery success and patient satisfaction. In the past, assessments of the IOL decentration and tilt have been conducted using the ultrasound biomicroscopy, Purkinje meter, anterior segment analyzer (e.g., Pentacam), wavefront aberrometry (e.g., OPD-SCAN Ш), or anterior segment OCT. The Purkinje meter is the only method that provides direct evaluation of decentration and tilt however its repeatability has been described as inferior.17 Holladay et al.18 reported that the visual axis was the general standard for the IOL decentration and tilt measurement, and correlated well with CTA. In addition, Zhang et al.10 found CTA was the best reference for the IOL decentration and tilt compared with the pupillary and optical axis. As a novel SS-ОСТ, CASIA2 is the first to evaluate the decentration and tilt using the СТА as a reference. In addition, this device is advantaged by its faster scanning speeds, deeper scanning depths, and higher scanning resolutions. Direct assessment of decentration and tilt by CASIA2 can reduce the bias caused by secondary processing. Therefore, in this study we evaluated the repeatability of CASIA2 in measuring the decentration and tilt of both the crystalline lens and IOL in cataract patients, as well as the effects of pupil size on the measurements.Janunts et al.19 found Purkinje meter measurements for IOL decentration and tilt under non-mydriatic conditions to have excellent repeatability. Ding et al.20 found anterior segment OCT had better repeatability compared with the Purkinje meter or the Pentacam. Sato et al.21 used CASIA2 to evaluate the IOL decentration and tilt in 50 cataract patients and found high repeatability of one-piece and three-piece IOL measurements. Previous studies demonstrated that anterior segment OCT has clear advantages in measuring IOL decentration and tilt. The current study assessed CASIA2’s repeatability through ICC, TRT, and CoV for crystalline lens and IOL decentration and tilt. While it performed well on most parameters, poor repeatability of crystalline lens decentration was noted. This may be partly explained by severe lens opacities, poor fixation, measurement errors, and an unclear outline on image capture.
Schaeffel et al.22 found the crystalline lens decentered approximately 0.3 mm downward relative to the pupil center when using a Purkinje meter and another found crystalline lens decentered 0.25 mm toward the temporal direction.23 Kimura et al.24 used CASIA2 to measure the crystalline lens and IOL in 100 cataract eyes and found crystalline lens and IOL decentration was directed temporally with average range of 0.03–0.12 mm, and tilted inferotemporally 4.22°–5.30° using CTA as a reference. Sato et al.21 assessed one-piece and three-piece IOL decentration and tilt using CASIA2 at 3 hours, 24 hours, 2 weeks, and 4 weeks after cataract surgery, but decentration was unspecific and tilted inferotemporally. Chen et al assessed IOL of 196 cataract eyes in China25 and reported average decentration was 0.21 mm and 0.20 mm before and after mydriasis, respectively, whilst tilt was 4.22° and 4.89°. These findings suggest IOL decentration direction is inconsistent, however tilt is consistently directed inferotemporally in both eyes. This study discovered crystalline lens decentered and tilted inferotemporally before and after mydriasis in a symmetric manner. This finding proved that the eyes were tilted relative to the optical axis when they were aligned along the visual axis. Under non-mydriatic and mydriatic conditions, the right IOL decentered toward inferior direction. In contrast, left IOL decentered inferotemporally. Gravity may influence this decentration inferiorly, however horizontal decentration may be caused by unstable positioning of IOL in the early postoperative period. In line with previous findings, we discovered both right and left IOLs tilted inferotemporally before and after mydriasis in a symmetric manner. This study found a mean decentration of 0.2 mm and a mean tilt of 5° in crystalline lenses and IOL. The magnitude of decentration in this study is therefore consistent with Chen et al.25, but greater than Kimura et al.24 In contrast, tilt magnitude was comparable to Kimura et al.24 but greater than Chen et al.25
The present study found crystalline lens and IOL decentration and tilt before and after mydriasis were significantly correlated. Moreover, no statistically significant differences between non-mydriatic and mydriatic conditions for the decentration and tilt of crystalline lens and IOL were noted which suggests pupil shape and size does not affect the accuracy of CASIA2 for these functions. Therefore, this study suggests CASIA2 is a feasible and convenient method for measuring the decentration and tilt of crystalline lenses and IOL without mydriasis in clinical settings.
Despite the insights of our findings, some limitations should be acknowledged. First, in addition to repeatability, reproducibility is a crucial indicator for assessing the accuracy of an instrument however this was not investigated by this study. Future studies should seek to determine this outcome for decentration and tilt in both crystalline lens and IOL. Secondly, there was no classification for lens opacities in each patient, therefore degree of cataract could introduce bias to our findings. Finally, the consistency of CASIA2 with other classical devices in measuring crystalline lens and IOL decentration and tilt was not evaluated, which inhibits the accuracy of CASIA2 from being properly assessed.
In conclusion, decentration and tilt of crystalline lenses in both eyes were directed inferotemporally, while in right eyes, IOL decentration was concentrated inferiorly and tilted inferotemporally, and decentered and tilt was inferotemporal in left IOL eyes. This study found CASIA2 to be a repeatable instrument for assessing the decentration and tilt of IOL and crystalline lenses under mydriatic and non-mydriatic conditions, but not for the magnitude of crystalline lens decentration. There were no significant differences in the decentration and tilt of crystalline lens and IOL, and significant correlations were observed between mydriatic and non-mydriatic conditions. Therefore, CASIA2 may be used under non-mydriatic condition in clinical practice.
Disclosures: The authors have no conflicts of interest concerning this study.
Author contributions: Tang Yuling: conducting the study; acquisition, analysis, or interpretation of data; and drafting of the manuscript. Liao Xuan: study concept and design; and technical guidance. Tan Qingqing: study concept and design; guiding analysis of data. Qian Jiulin, Yang Li, Zhou Guimei: conducting the study and acquisition of data. Lan Changjun: study concept and design; and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
[1]Pérez-Merino P, Marcos S. Effect of intraocular lens decentration on image quality tested in a custom model eye[J]. J Cataract Refract Surg, 2018, 44(7):889-896. DOI: 10.1016/j.jcrs.2018.02.025.
[2]Lawu T, Mukai K, Matsushima H, et al. Effects of decentration and tilt on the optical performance of 6 aspheric intraocular lens designs in a model eye[J]. J Cataract Refract Surg, 2019, 45(5):662-668. DOI: 10.1016/j.jcrs.2018.10.049.
[3]兰长骏, 唐玉玲, 廖萱.人工晶状体的偏心和倾斜[J].中华眼科杂 志, 2021, 57(7):552-556. DOI: 10.3760/cma.j.cn112142-20210223-00096.
[4]Wang HL, Liu G, Jia WC. Application of capsular tension ring implantation during phacoemulsification for ultra-high myopia complicated with cataract[J]. Chin J Exp Ophthalmol, 2020, 38(2):114-120. DOI:10.3760/cma.j.issn.2095-0160.2020.02.007.
[5]Weikert MP, Golla A, Wang L. Astigmatism induced by intraocular lens tilt evaluated via ray tracing[J]. J Cataract Refract Surg ,2018,44(6): 745 — 749. DOI: 10. 1016/j.jcrs.2018. 04. 035.
[6]Chansangpetch S, Nguyen A, Mora M, et al. Agreement of anterior segment parameters obtained from swept-source Fourier-domain and time-domain anterior segment optical coherence tomography[J]. Invest Ophthalmol Vis Sei, 2018, 59(3):1554-1561. DOI: 10.1167/iovs.17-23574.
[7]Zhong X, Long E, Chen W, et al. Comparisons of the in-the-bag stabilities of single-piece and three-piece intraocular lenses for age- related cataract patients: a randomized controlled trial[J/OL]. BMC Ophthalmol, 2016, 16:100[2021-07-10]. http://www.ncbi.nlm.nih.gov/puhmed/27392024. DOI: 10.1186/sl2886-016-0283-4.
[8] Li SF, Zhang XSn, You CT, et al. The various axes and angles of the human eye and their application in refractive surgery[J]. Chin J Optom Ophthalmol Vis Sci, 2020, 22(8):637-640. DOI: 10.3760/cma.j.cn115909-20190504-00130.
[9]Ashena Z, Maqsood S, Ahmed SN, et al. Effect of intraocular lens tilt and decentration on visual acuity, dysphotopsia and wavefront aberrations[J/OL]. Vision(Basel), 2020, 4(3):41[2021-07-10]. http://www.ncbi.nlm.nih.gov/puhmed/32937750. DOI: 10.3390/vision4030041.
[10]Zhang F, Zhang J, Li W, et al. Correlative comparison of three ocular axes to tilt and decentration of intraocular lens and their effects on visual acuity[J]. Ophthalmic Res, 2020, 63(2):165-173. DOI: 10.1159/000504716.
[11]McAlinden C, Khadka J, Pesudovs K. Precision (repeatability and reproducibility) studies and sample-size calculation[J]. J Cataract Refract Surg, 2015, 41(12):2598-2604. DOI: 10.1016/j.jers.2015.06.029.
[12]McAlinden C, Khadka J, Pesudovs K. Statistical methods for conducting agreement (comparison of clinical tests) and precision (repeatability or reproducibility) studies in optometry and ophthalmology[J]. Ophthalmic Physiol Opt, 2011, 31(4):330-338. DOI: 10.1111/j.1475-1313.2011.00851.X.
[13]Bland JM, Altman DG. Measuring agreement in method comparison studies[J]. Stat Methods Med Res, 1999, 8(2):135- 160. DOI: 10. 1177/096228029900800204.
[14]Gobbe M , Guillon M, Maissa C. Measurement repeatability of corneal aberrations[J].J Refract Surg, 200 , 18(5):S567-S571. DOI: 10.3928/1081-597X-20020901-14.
[15]Müller R, Büttner P. A critical discussion of intraclass correlation coefficients[J].Stat Med, 1994, 13(23-24):2465-2476. DOI: 10.1002/sim.4780132310.
[16]Holladay JT, Dudeja DR, Koch DD. Evaluating and reporting astigmatism for individual and aggregate data[J] .J Cataract Refract Surg, 1998, 24(1) 57-65. DOI: 10. 1016/s0886-3350(98)80075-8.
[17]Maedel S, Hirnschall N, Bayer N, et al. Comparison of intraocular lens decentration and tilt measurements using 2 Purkinje meter systems[J]. J Cataract Refract Surg, 2017, 43(5):648-655. DOI: 10.1016/j.jers.2017.01.022.
[18]Holladay JT, Calogero D, Hilmantel G, et al. Special report: American Academy of Ophthalmology task force summary statement for measurement of tilt, decentration , and chord length[J]. Ophthalmology, 2017, 124(1):144-146. DOI: 10.1016/j.ophtha.2016.09.030.
[19]Janunts E,Chashchina E, Seitz B, et al. Reliability of a single light source Purkinjemeter in pseudophakic eye[J]. Optom Vis Sei, 2015, 92(8):884-891. DOI: 10.1097/OPX.0000000000000644.
[20]Ding X , Wang Q, Chang P , et al. The repeatability assessment of threedimensional capsule-intraocular lens complex measurements by means of high-speed swept-source optical coherence tomography[J/OL]. PLoS One, 2015, 10(1):e0l42556 [2021-07-16]. http://www. ncbi.nlm.nih.gov/puhmed/26600254. DO: 10.1371/journalpone.0142556.
[21]SatoT, Shibata S, Yoshida M, et al. Short-term dynamics after single- and three-piece acrylic intraocular lens implantation: a swept-source anterior segment optical coherence tomography study [J/OL]. Sei Rep, 2018, 8(1):10230[2021-08-26]. http://www.ncbi.nlm.nih.gov/pubmed/29980770. DOI: 10. 10.1038/s41598-018-28609-1.
[22]Schaeffel F. Binocular lens tilt and decentration measurements in healthy subjects with phakic eyes[J] .Invest Ophthalmol Vis Sci, 2008, 49(5):2216-2222. DOI:10.1167/iovs.07-1022.
[23]Hu CY,Jian JH, Cheng YP , et al. Analysis of crystalline lens position[J]. J Cataract Refract Surg, 2006, 32(4):599-603. DOI: 10.1016/ j.jcrs.2006.01.016.
[24]Kimura S, Morizane Y, Shiode Y, et al. Assessment of tilt and decentration of crystalline lens and intraocular lens relative to the corneal topographic axis using anterior segment optical coherence tomography[J/OL]. PLoS One, 2017, 12(9):e0l84066[2021-0826]. http://www.ncbi.nlm.nih.gov/puhmed/28863141. DOI: 10.1371/journalpone.0184066.
[25]Chen X,Gu X, Wang W, et al. Characteristics and factors associated with intraocular lens tilt and decentration after cataract surgery[J].J Cataract Refract Surg, 2020, 46(8):1126-1131. DOI: 10.1097/j. jcrs.0000000000000219.
[26]Chang DH, Waring GO IV. The subject-fixated coaxially sighted corneal light reflex: a clinical marker for centration of refractive treatments and devices[J]. Am J Ophthalmol, 2014, 158 (5):863-874. DOI: 10.1016/j.ajo.2014.06.028.