Abstract [View PDF] [Read Full Text]
Objective
To evaluate the efficacy and safety of corneal bandage lens in the treatment of dry eye after cataract surgery in patients with mild meibomian gland dysfunction (MGD).
Methods
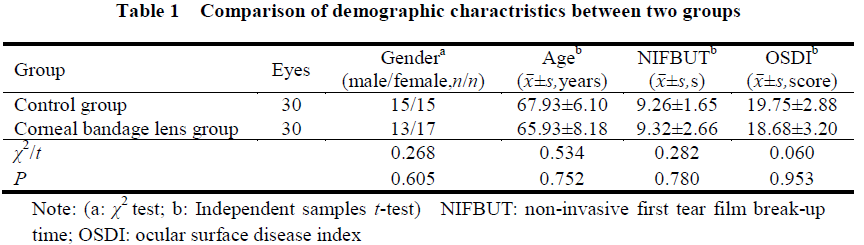
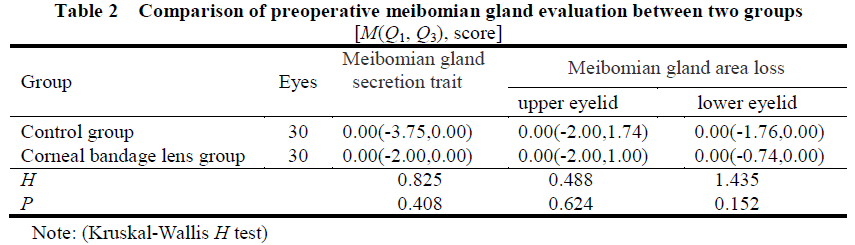
A non-randomized controlled clinical study was conducted.Sixty eyes of 60 patients with mild MGD after cataract surgery were enrolled in Yantai Yuhuangding Hospital from June 2020 to February 2021.The patients were divided into bandage lens group and control group according their willingness, with 30 eyes in each group.All the patients received phacoemulsification and intraocular lens implantation and were administered with the same postoperative medication.Patients in bandage lens group wore lenses for 14 days continuously after the operation.Patients in control group did not wear the corneal bandage lens after the operation.The structure and inflammation of the anterior segment were observed with a slit-lamp microscope before operation and on days 1, 7, and 14 after the operation.Best corrected visual acuity (BCVA) was obtained using a standard logarithmic visual acuity chart.Ocular surface symptoms were evaluated via an ocular surface disease index (OSDI) questionnaire.The intraoperative changes of meibomian glands were assessed with an ocular surface analyzer and the non-invasive first tear film break-up time (NIFBUT) was recorded.Corneal epithelium defects were observed by corneal fluorescein sodium staining (CFS). This study adhered to the Declaration of Helsinki and was approved by an Ethics Committee of Yantai Yuhuangding Hospital (No.2021-363). Written informed consent was obtained from each patient before any medical examination.
Results
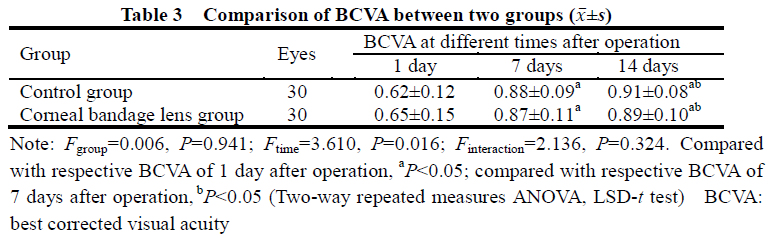
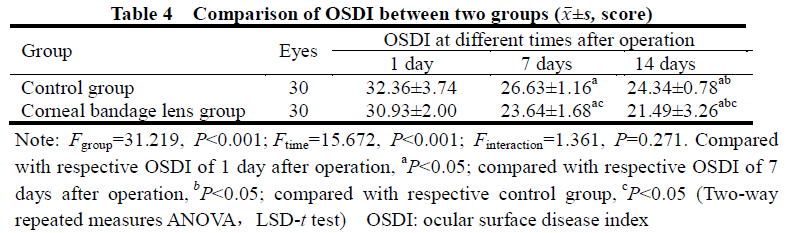
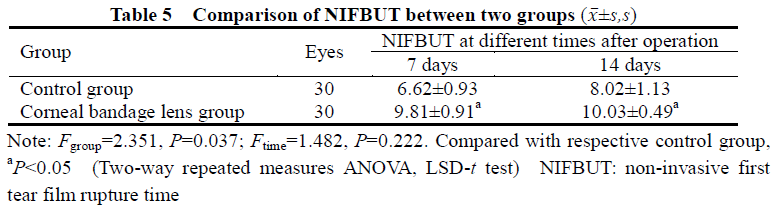
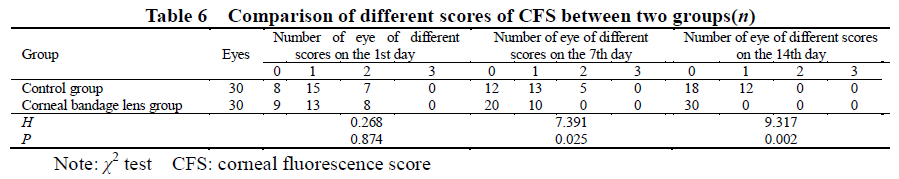
On the 1st, 7th, and 14th day after surgery, no inflammatory reaction or complication was observed in both groups.Statistically significant differences in BCVA among different postoperative time points were found (Ftime=3.610, P=0.016). BCVA on the 7th day after surgery were higher than that on the 1st day after surgery, and the BCVA on the 14th day after surgery were significantly higher than those on the 1st and 7th day after surgery in both groups, with statistically significant differences (all at P<0.05). There were statistically significant differences in OSDI scores between the two groups at different postoperative time points (Fgroup=31.219, P<0.001; Ftime=15.672, P<0.001). The OSDI scores of bandage lens group were significantly lower than those of control group on the 7th and 14th day after surgery, OSDI scores in both groups on the 14th day after surgery were significantly lower than those on the 1st and 7th day after surgery, with statistical significance (all at P<0.05). The NIFBUT values on the 7th and 14th day after surgery were (6.62±0.93)s and (8.02±1.13)s, in control group, bandage lens group and (9.81±0.91)s and (10.03±0.49)s in bandage lens group, with a statistically significant difference between them (Fgroup=2.351, P=0.037), and the NIFBUT values of bandage lens group on the 7th and 14th day after surgery were higher than those of control group, with statistically significant differences (both at P<0.05). The number of high CFS score eyes of bandage lens group were lower than those of control group on the 7th and 14th day after surgery, and the differences were statistically significant (χ2=7.391, P=0.025; χ2=9.317, P=0.002).
Conclusions
For patients with mild MGD after cataract surgery, wearing bandage contact lens has no obvious ocular adverse reaction and can promote the growth of corneal epithelium, enhance the stability of tear film, improve dry eye symptoms, and relieve dry eye manifestations after surgery.
Key words:
Figures and tables
Contributor Information
School of Clinical Medicine, Weifang Medical University, Weifang 261053, China
Department of Ophthalmology, Yantai Yuhuangding Hospital Affiliated to Qingdao University, Yantai 264000, China
Department of Ophthalmology, Yantai Yuhuangding Hospital Affiliated to Qingdao University, Yantai 264000, China